Einige wesentliche Aufsätze haben wir ins Deutsche übersetzt, ebenso einen großen Teil der Hilfen zur Bewertung der diagnostischen Methoden.
Lose Einzelheiten haben wir im Lexikon gesammelt.
| Über das hier angebotene Material hinaus können wir zur Zeit Ihre persönlichen Fragen nur noch gegen Beteiligung an den laufenden Kosten dieser Website beantworten. |
Rückfallfreie Zeit nach einer als MS fehldiagnostizierten NeuroborrelioseWarum zuerst experimentell gegen Neuroborreliose behandelt wurde - und wie.Interpretation in: Rückfallfreie Zeit (Stand 26. Juni 2021):
|
| Lymenet.de
- Home
Neues
auf Lymenet.de
Über
Lyme-Borreliose
Hintergrund und medizinische Fachliteratur
Berichte über Tagungen und Info-Veranstaltungen Lyme-Aktivismus, Ethik, Menschenrechte Beiträge von Selbsthilfegruppen Beiträge in Zeitschriften, Radio und TV
Hinweise
zum Offline-Lesen
|
|
Version: 12. Juli 2021 Adresse dieser Seite Joachim Gruber |
Neuigkeiten - Bekanntmachungen
(Datum: 10. Juli 2021)
Unmittelbar nach einem Zeckenstich ist es empfehlenswert, Borrelien-IgG-Antikörper- und Borrelien-IgM-Antikörper Immunoblots (Western Blots) machen zu lassen. Damit wird der (gesunde) Status festgehalten, der vor der Immunreaktion auf die Infektion bestand. Wenn dann später Symptome auftreten, kann man bei einem erneuten Western Blot die Immunreaktion als Veränderungen gegenüber dem gesunden Status besser erkennen.
Beim gesunden Status bekommt vom ausführenden Labor die Nachricht:
- "Borrelien IgG-Ak (Immunoblot) negativ",
- "Borrelien IgM-Ak (Immunoblot) negativ".
 zum Vergrößern auf Bild klicken
zum Vergrößern auf Bild klicken
|
Mit dem Western Blot soll nach folgenden "Banden" gesucht werden:
|
(Datum: 4.Oktober 2020)
Nengyin Liu1, Ruth R. Montgomery1, Stephen W. Barthold2 and Linda K. Bockenstedt1, Myeloid Differentiation Antigen 88 Deficiency Impairs Pathogen Clearance but Does Not Alter Inflammation in Borrelia burgdorferi-Infected Mice,
INFECTION AND IMMUNITY, June 2004, p. 3195-3203
1 Department of Internal Medicine, Yale University School of Medicine, New Haven, Connecticut,
2Center for Comparative Medicine, Schools of Medicine and Veterinary Medicine, University of California at Davis, Davis, California
Inflammation, Innate immunity, Toll like receptor signaling, Biological Sciences, Infection and immunity
The spirochete Borrelia burgdorferi causes acute inflammation in mice that resolves with the development of pathogen-specific adaptive immunity.
suggesting the involvement of other TLRs or non-TLR mechanisms in the induction of acute inflammation.
For this study, we used mice that were deficient in the intracellular adapter molecule myeloid differentiation antigen 88 (MyD88), which is required for all TLR-induced inflammatory responses, to determine whether the interruption of this pathway would alter B. burgdorferi-induced disease.
- Infected MyD88 mice developed carditis and arthritis, similar to the disease in wild-type (WT) mice analyzed at its peak (days 14 and 28) and during regression (day 45).
- MyD88 macrophages produced tumor necrosis factor alpha only when spirochetes were opsonized, suggesting a role for B. burgdorferi-specific antibody in disease expression.
- MyD88 mice produced stronger pathogen-specific Th2-dependent immunoglobulin G1 (IgG1) responses than did WT mice, and their IgM titers remained significantly elevated through 90 days of infection.
- Despite specific antibodies, the pathogen burden was 250-fold higher in MyD88 mice than in WT mice 45 days after infection; by 90 days of infection, the pathogen burden had diminished substantially in MyD88 mice, but it was still elevated compared to that in WT mice.
- The elevated pathogen burden may be explained in part by the finding that MyD88 peritoneal macrophages could ingest spirochetes but degraded them more slowly than WT macrophages.
(Datum: 11.September 2020)
CONCLUSIONS
(Datum: 22. Juni 2020)
Wer diese Krankheit in dieser langwierigen chronischen Form nicht selbst erlebt hat, wird sie auch nicht authentisch nachempfinden können. Deshalb hat wohl die Medizin, Politik und Justiz auf diesem Gebiet bislang nicht die notwendigen Erfolge gebracht..
(Datum: 21. April 2019)
The Situation of Human Rights Defenders of Lyme and Relapsing Fever Borreliosis,
(Datum: 30. Januar 2019)
"Dreh-und Angelpunkt des Streites um die (Neuro-) Borreliose ist die Frage, ob es nach einer Behandlung eine Erregerpersistenz geben kann, die die betroffenen Menschen krank macht. Hierzu gibt es 3 neuere Studien, 2 an Rhesus Makaken und eine an Menschen, die belegen, dass es trotz einer (28-tägigen) Behandlung zu Persistern kommen kann:
Auszug aus der Slide-Show zur Neuroborreliose-Leitlinie
Ist die Leitlinie zur Neuroborreliose eine S3-Leitlinie?
Ausblick: Wir benötigen
(Datum: 23. Januar 2019)
Der Ausschuss des Parlaments, der sich speziell mit LB auseinandersetzt, trägt den Namen "Umweltfragen, öffentliche Gesundheit und Lebensmittelsicherheit" (ENVI).
Ich halte es für dringend nötig, dass möglichst viele von uns sich rasch an sämtliche ENVI-Mitglieder wenden und ihre Hauptanliegen vorbringen. Am besten auch Evidenz basierte Literatur, etc., etc., so dass wir dokumentieren, dass eigentlich ein gewaltiges Wissen vorhanden ist, jedoch (noch) unterdrückt wird.
Wir müssen rasch einen Durchbruch erreichen - bitte helfen Sie mit.
Ich meinerseits habe dies bereits getan, doch da die Schweiz kein EU-Mitglied ist, weiss ich nicht, ob meine Anliegen berücksichtigt werden.
Sehr geehrter Herr Barjenbruch,
Viele Aktivitäten zur Aufklärung (auch von den verschiedenen Patienten-Organisationen >Google) und Hinweise auf ein dringend notwendiges adäquates Borreliose-Therapieprogramm und entsprechende Borreliose-Zentren waren bislang über Jahre mit wenig Erfolg beschieden.
Die Hintergründe dieses für die vielen Borreliose-Betroffenen leidvollen Dilemmas kommen aus den USA von der
Lyme Disease - Infectious Diseases Society of America (IDSA)
und deren Doktrin, dass Borreliose mit 3 Wochen Antibiotika leicht behandelbar ist und es prinzipiell keine chronische Borreliose gibt. Diese sind vom Nationalen Referenzzentrum für Borreliose (NRZ), München (Dr. Fingerle) übernommen worden und in den Leitlinien für Borreliose mit Federführung von Prof. Rauer (Freiburg) manifestiert, woran sich überwiegend die Ärzte orientieren und entsprechend leider falsch behandeln.
Dem gegenüber steht die International Lyme and Associated Diseases Society (ILADS), deren wissenschaftlich belegten und von praktizierenden Ärzten bestätigten Thesen, die chronische Borreliose existiere massenhaft und sei mit Langzeit-Antibiotika zu behandeln. Dazu hat die Deutsche Borreliose-Gesellschaft (DBG) entsprechende Leitlinien erstellt, die jedoch aufgrund der IDSA-Doktrin in der Praxis zum Schaden der Patienten leider nicht generell die entsprechend notwendige Anerkennung finden.
Die genaueren Hintergründe sind beschrieben in dem Buch "Die verschwiegene Epidemie" von Birgit Jürschik-Busbach (ISBN: 978-3-981-41050-1).
Zwischen diesem Expertenstreit stehen die Betroffenen nun schon über 30 Jahren oftmals mit wenig Hoffnung auf Gesundung, und aus purer Verzweiflung finden immer wieder schwer Borreliose-Geschädigte nur den Ausweg im Suizid (s. Berichte Betroffener). (weiterlesen) Info von Corry Welker (Teil A in Bericht Januar 2019)
Die Studien
(Datum: 6. August 2018) Marianne J. Middelveen,1 Eva Sapi,2 Jennie Burke,3 Katherine R. Filush,2 Agustin Franco,4 Melissa C. Fesler,5 and Raphael B. Stricker5,*, Persistent Borrelia Infection in Patients with Ongoing Symptoms of Lyme Disease, Healthcare, 14 April 2018 (Auszüge in deutsch von Uta Everth) 1 Atkins Veterinary Services, Calgary, AB T3B 4C9, Canada; ten.sulet@leddim
Introduction: Lyme disease is a tickborne illness that generates controversy among medical providers and researchers. One of the key topics of debate is the existence of persistent infection with the Lyme spirochete, Borrelia burgdorferi, in patients who have been treated with recommended doses of antibiotics yet remain symptomatic. Persistent spirochetal infection despite antibiotic therapy has recently been demonstrated in non-human primates. We present evidence of persistent Borrelia infection despite antibiotic therapy in patients with ongoing Lyme disease symptoms.
Methods: In this pilot study, culture of body fluids and tissues was performed in a randomly selected group of 12 patients with persistent Lyme disease symptoms who had been treated or who were being treated with antibiotics. Cultures were also performed on a group of ten control subjects without Lyme disease. The cultures were subjected to corroborative microscopic, histopathological and molecular testing for Borrelia organisms in four independent laboratories in a blinded manner.
Results: Motile spirochetes identified histopathologically as Borrelia were detected in culture specimens, and these spirochetes were genetically identified as Borrelia burgdorferi by three distinct polymerase chain reaction (PCR)-based approaches. Spirochetes identified as Borrelia burgdorferi were cultured from the blood of seven subjects, from the genital secretions of ten subjects, and from a skin lesion of one subject. Cultures from control subjects without Lyme disease were negative for Borrelia using these methods.
Conclusions: Using multiple corroborative detection methods, we showed that patients with persistent Lyme disease symptoms may have ongoing spirochetal infection despite antibiotic treatment, similar to findings in non-human primates. The optimal treatment for persistent Borrelia infection remains to be determined.
Schlussfolgerungen: Mit Hilfe von mehreren einander bestätigenden Nachweisverfahren konnten wir zeigen, dass Patienten mit persistierenden Borreliose-Symptomen trotz Behandlung mit Antibiotika eine weiterhin bestehende Infektion mit den Spirochäten haben können, ähnlich wie es bei nicht-menschlichen Primaten gefunden wurde. Die optimale Behandlung einer Borreliose-Infektion muss noch gefunden werden.
Link: The Microbiology Information Portal, Lyme disease
In der Spätphase ist es nicht möglich, zwischen Krankheitsmanifestationen des Spätstadiums oder einer chronischen Borreliose zu unterscheiden. Dies ist auch aufgrund pathophysiologischer Überlegungen nicht zu erwarten, da es sich in beiden Fällen um eine persistierende generalisierte Infektion mit Borrelien handelt.
... Da das Erythema migrans als pathognomonisches und krankheitsbeweisendes Phänomen, also in etwa 30-50 % der Fälle nicht auftritt oder nicht festgestellt wird, muss sich die Diagnose auf die übrigen Symptome der Borreliose stützen. Bezüglich der vielfältigen Symptomatik der Borreliose sei wiederum auf Tabelle 7 (nach Sigal (4)) und Tabelle 9 (nach ILADS (3)) verwiesen.
Die Deutsche Borreliose-Gesellschaft hat eine Übersicht über die Symptomatik der Borreliose zusammengestellt und die vielfältigen Krankheitsmanifestationen nach Organsystemen geordnet. Diese Übersicht enthält die Tabelle 9a, Seite 18). Die Übersicht stützt sich auf Angaben von Ärzten der Deutschen Borreliose-Gesellschaft unter Einbeziehung verschiedener Literaturquellen. ...
1. Lyme Bacteria Hides Inside Parasitic Worms, Causing Chronic Brain Diseases
... MacDonald found two Borrelia pathogens, including B. burgdorferi the causative agent of Lyme disease, thriving inside parasitic nematode worms, worm eggs or larvae in the brain tissue of nineteen deceased patients. These microscopic worms are endosymbionts, meaning the Borrelia bacteria dwell inside the worms. A tick bite delivers the nematode into the human body.
... The Rocky Mountain Multiple Sclerosis Center Tissue Bank provided MacDonald with ten specimens from deceased MS patients; all ten specimens showed evidence of Borrelia infected nematodes. ... (see below: A. MacDonald's London Lecture, May 15, 2016, Borrelia Burgdorferi Group Spirochetes Detected in Blood and Cerebrospinal Fluid - in Seronegative Patients (ELISA and Western Blot USA and Europe))
Herein is described image based evidence for the detection of cerebrospinal fluid infection/infestation with worms, probably vectored by ixodid ticks (Ref. 3), to produce nematode filarial CSF infection which is followed by worm [nematode filarial] invasion of the brain solid tissue to produce areas of myelin destruction, which typify the clinical and pathological signatures of Multiple Sclerosis in the human host. It is herein proposed, that the worms enter the deep brain white matter regions via direct extension from CSF worm infestations, and that worms slough their outer sheath tissues as detritus. A cascade of host responses which terminates in the destruction of axonal myelin, and entire brain neural and glial elements produces Multiple Sclerosis. Further host insult by the invading worms in deep brain white matter ensues from the comet like trail of nematode filarial eggs and zygotes in brain tissue. Collectively, the worm foreign material terminates in a host response which destroys the native architecture of the white matter. The inciting worm in brain tissue may not be evident at autopsy, because the worms may either have died or moved to a new topographical site remote from the plaques.
3. Lyme Bacteria Hides Inside Parasitic Worms, Causing Chronic Brain Diseases
... The Rocky Mountain Multiple Sclerosis Center Tissue Bank provided MacDonald with ten specimens from deceased MS patients; all ten specimens showed evidence of Borrelia infected nematodes. Infected worms were also found in five tissue specimens from patients who succumbed to the highly malignant brain tumor Glioblastoma multiforme, the same cancer which took the life of Senator Edward Kennedy (D-MA). Ironically, in 1993, Senator Kennedy chaired a hearing of the Labor and Human Resources committee titled: Lyme disease: A Diagnostic and Treatment Dilemma. Finally, four specimens from patients who died from Lewy Body dementia, the same illness which afflicted comedian Robin Williams, also showed the presence of infected nematodes.
4. Alan B. MacDonald, Borrelia Burgdorferi Group Spirochetes Detected in Blood and CSF in (ELISA & Western Blot) Seronegative Patients,
Slides:
Monica E. Embers, Nicole R. Hasenkampf, Mary B. Jacobs, Amanda C. Tardo, Lara A. Doyle-Meyers, Mario T. Philipp, Emir Hodzic, Variable manifestations, diverse seroreactivity and post-treatment persistence in non-human primates exposed to Borrelia burgdorferi by tick feeding, PLoS ONE 12(12): e0189071, Dec. 13, 2017.
Nicholas A. Crossland, Xavier Alvarez, Monica E. Embers, Late Disseminated Lyme Disease: Associated Pathology and Spirochete Persistence Post-Treatment in Rhesus Macaques, The American Journal of Pathology 2791, 16 Nov. 2017
Filmtipp: Götter in Weiß, 15.11.2017 | 88 Min. | UT | Verfügbar bis 15.12.2017 in ard-Mediathek (Wertung in Ärztezeitung: Klinikärzte im Konflikt)
(Washington, DC) The examination of autopsied brain tissues from patients who died of serious neurological conditions has revealed that many tick-borne infections, such as Lyme disease, go undiagnosed and untreated. Board-certified pathologist, Alan B. MacDonald, MD, says his research shows "tick infections are not easily detected with routine tests, nor are they easily cured with short courses of antibiotics.Ó
MacDonald will present his findings Thursday on Capitol Hill, in the Rayburn House Office Building, at a forum to explore the scientific, economic, and policy challenges posed by the epidemic of Lyme disease and associated tick-borne illnesses.
MacDonald found three Borrelia pathogens, including B. burgdorferi the causative agent of Lyme disease, thriving inside parasitic nematode worms, worm eggs or larvae in the brain tissue of nineteen deceased patients. These microscopic worms are endosymbionts, meaning the Borrelia bacteria dwell inside the worms. A tick bite delivers the nematode into the human body.
At the Dr. Paul Duray Research Fellowship Endowment Inc., pathologist Alan MacDonald MD, FCAP, FASCP, has been using highly specific Molecular Beacon DNA probes to in-vestigate the role of Borrelia in neurological diseases. The results have been no less than astonishing.
Using the technique of Fluorescent in situ hybridization (FISH), Borrelia biofilms (both Borrelia burgorferi and relapsing-fever typeŃmiyamotoi) have been repeatedly detected in antibody-negative patients, as well as in patients treated with antibiotics.
In May 2016, the Duray foundation discovered that Borrelia endosymbionts dwell inside parasitic nematode worms which invade brain tissue, trampling neurons, and leaving a trail of destruction in their wake. Endosymbionts live in harmony with their nematode host, but cause devastation once released into the brain.
Costs for the Lyme disease group might be expected to be higher, particularly if expensive long term intravenous antibiotics were used, a practice that has been reported in the treatment of the more heterogeneous and complex group of patients with long term chronic symptoms where Lyme disease may not be the sole cause of illness. [26] However, we did not find increased costs associated with IV antibiotics in our study population [S3 and S4 Tables].
Welche finanziellen Auswirkungen hat die Lyme-Borreliose auf das amerikanische Gesundheitswesen?
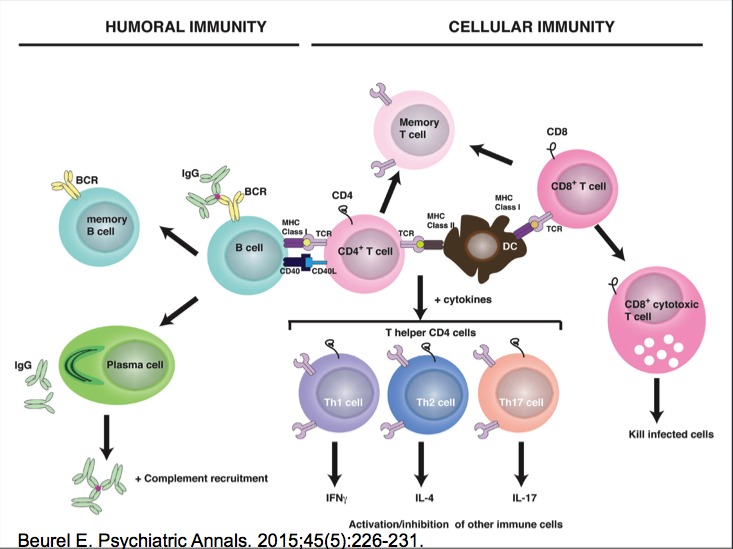
Our recent studies suggested that germinal center responses were nonfunctional after primary B. burgdorferi infection, as long-lived antibody-secreting plasma cells and memory B cells were not induced for months after infection.
... while affinity maturation of antibodies against a prototypic T-dependent B. burgdorferi protein, Arthritis-related protein (Arp), were initiated, these increases were reversed later, coinciding with the previously observed involution of germinal centers. The cessation of affinity maturation was not due to the appearance of inhibitory or exhausted CD4 T cells or a strong induction of regulatory T cells. In vitro T-B cocultures demonstrated that T cells from B. burgdorferi-infected ... mice supported the rapid differentiation of B cells into antibody-secreting plasma cells rather than continued proliferation, mirroring the induction of rapid short-lived instead of long-lived T-dependent antibody responses in vivo. The data further suggest that B. burgdorferi infection drives the humoral response away from protective, high-affinity, and long-lived antibody responses and toward the rapid induction of strongly induced, short-lived antibodies of limited efficacy.
Previous studies have demonstrated that B. burgdorferi infection induces predominantly T-independent B cell responses, potentially explaining some of these findings. However, others have shown effects of T cells on the isotype profile and the magnitude of the B. burgdorferi-specific Abs.
This study aimed to further investigate the humoral response to B. burgdorferi and its degree of T cell dependence, with the ultimate goal of elucidating the mechanisms underlying the failure of effective immunity to this emerging infectious disease agent. Our study identifies distinct stages in the B cell response using a mouse model, all marked by the generation of unusually strong and persistent T-dependent and T-independent IgM Abs.
Wenn Sie selbst an dieser Umfrage teilnehmen möchten, klicken Sie hier.
The definitive experimental data indicate transmission of LD spirochetes in <16 hours and frequently in <24 hours. No studies have been carried out to characterize transmission with attachment times of <16 hours and some did not report any data for <36 hours. The animal studies, however, did not comprehend significant variables such as the presence of spirochetes within the salivary glands at the start of feeding, nor the effect of delayed attachment once a tick adheres to a host. Both of these will reduce the time for infectious spirochetes to invade the host compared to the model that requires a change from dormancy to active migration from the midgut to the salivary glands and then to the host. Also, co-feeding and partial feeding of ticks with displacement from companion animals to humans must be considered a factor for rapid transmission of LD. "
Discussion:
According to this review, mind-body medicine had no effect on
This paper demonstrates that studies of mind-body techniques for treating MS symptoms are feasible, and that more stringently designed, well-executed research is needed in this population to determine efficacy.
Literature
P. Grossman, L. Kappos, H. Gensicke et al., "MS quality of life, depression, and fatigue improve after mindfulness training: a randomized trial," Neurology, vol. 75, no. 13, pp. 1141-1149, 2010.
B. S. Oken, S. Kishiyama, D. Zajdel et al., "Randomized controlled trial of yoga and exercise in multiple sclerosis," Neurology, vol. 62, no. 11, pp. 2058-2064, 2004.
D. McClurg, R. G. Ashe, K. Marshall, and A. S. Lowe-Strong, "Comparison of pelvic floor muscle training, electromyog- raphy biofeedback, and neuromuscular electrical stimulation for bladder dysfunction in people with multiple sclerosis: a randomized pilot study," Neurourology and Urodynamics, vol. 25, no. 4, pp. 337-348, 2006.
First, the model is broken down into the three I's:
1. Infection,
2. Immune dysfunction, and
3. Inflammation.
Bacterial infections include Lyme disease and other Borrelia species as well as other tick-borne infections like
I think the Powassan virus is going to be a big problem in the future. The Powassan infection rate in ticks in the Hudson Valley has risen from 1-2% to 5-6% in the past several years. It has a mortality rate between 15-30% and can be transmitted within 15 minutes of a tick bite. We therefore really need to emphasize prevention!"
...
... Infections are therefore affecting the underlying terrain of the body causing free radical oxidative damage to the cells, and causing imbalances in hormones and the autonomic nervous system. It's not sufficient to just treat the infections. We must repair the damage from the infections to get a person back into balance.
... During the history and physical, it's important to discuss the chief complaints in order to create a differential diagnosis, and focus testing and treatment on those symptoms. The Horowitz Lyme MSIDS Questionnaire is on page 34 in my book, and has a list of the most frequent symptoms seen with Lyme. This was formulated from a questionnaire that was developed by Dr. Burrascano years ago. We expanded the original questionnaire and weighted the answers, adding sections to evaluate the risk of Lyme and associated co-infections. ... Health care providers and patients can therefore use it [the MSIDS Questionnaire] with confidence as an initial screening tool to evaluate the risk of having a tick-borne disorder. This would be especially useful in the case of a patient who comes in with a medical illness such as
... If the patient complains of tingling, numbness and burning sensations (suggestive of neuropathy), I then would check for
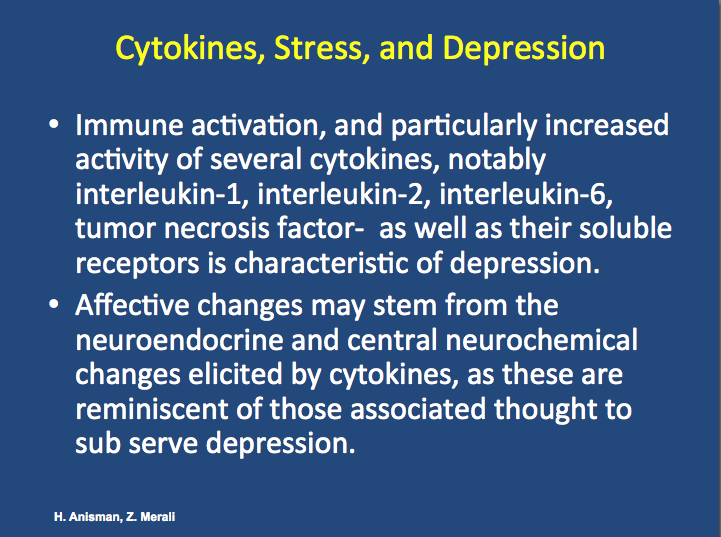
... Mind-body techniques and spirituality can be used as a tool to help heal patients with chronic disease. In the last chapter of my book I discuss some of the scientific studies on meditation. There's a lot of evidence that integrating meditation into a healing process can be helpful. Earlier on, we talked about how some inflammatory cytokines are causing people to remain ill with fatigue, joint pain, muscle pain, sleep disorders, memory problems, and psychiatric issues like anxiety and depression. With meditation, you can lower inflammatory cytokines. ...
... patients who have had this disease for many years have difficulty eradicating every last Borrelia organism (and parasites like Babesia). However, I don't feel it's necessary to eliminate every last organism. We live with many different bacteria and parasites. We need however to get the immune system to work properly and find a homeostatic balance with these organisms.
... I've used the MSIDS model effectively in thousands of patients who have been sick for a long time. The majority of people who come to see me have seen ten to 20 doctors before they come to my medical practice. I do help the majority of these people get better; some are a little bit better, some are moderately better, some are significantly better, and some become symptom free. The most important point in helping these patients is to look for points on the MSIDS model that have not been previously diagnosed and/or adequately treated ..."
According to the report, the ELISA and Western blot IgM tests, conducted as part of the autopsy, were positive for Borrelia burgdorferi, the agent that causes Lyme disease. Additional tests, including PCR (polymerase chain reaction) and immonohistochemistry (ICH) staining found Borrelia spirochete present in the patient's liver, heart, lung, and brain tissues.
"The findings support B. burgdorferi as the causative agent for his fulminant carditis and that the patient suffered fatal Lyme carditis," the authors write.
Joseph Elone, a high school honor roll student, had aspired to be an environmental engineer and loved the outdoors. He had just returned home from a two-week stay at a camp in Rhode Island, a state that is endemic for Lyme disease, when he fell ill. According to his parents, Joseph initially developed a mild cough, occasional fevers, a sore throat, malaise, headaches and body aches. Serology tests for Lyme disease and Anaplasmosis were negative."
Development of a Metabolic Biosignature for Detection of Early Lyme Disease, Clin Infect Dis. 2015 Mar 11.
Methods: Retrospective serum samples from patients with early Lyme disease, other diseases, and healthy controls were analyzed for small molecule metabolites by liquid chromatography-mass spectrometry (LC-MS). A metabolomics data workflow was applied to select a biosignature for classifying early Lyme disease and non-Lyme disease patients. A statistical model of the biosignature was trained using the patients' LC-MS data, and subsequently applied as an experimental diagnostic tool with LC-MS data from additional patient sera.
Metabolic biosignature development selected 95 molecular features that distinguished early Lyme disease patients from healthy controls. Statistical modeling reduced the biosignature to 44 molecular features, and correctly classified early Lyme disease patients and healthy controls with
Conclusion: The data provide proof-of-concept that metabolic profiling for early Lyme disease can achieve significantly greater (p<0.0001) diagnostic sensitivity than current two-tier serology, while retaining high specificity.
Der von der Schlichtungsstelle beauftragte Gutachter stellte fest: Eine Borreliose im Stadium I hat zweifelsfrei vorgelegen, dies sei
Für die Beurteilung sei davon auszugehen, daß zu Beginn der Kurbehandlung ein Insektenstich an der Wade vorgelegen hat, der von der Patientin bemerkt und von der behandelnden Schwester bestätigt wurde.
Das Vorliegen eines "Insektenstiches" gefolgt von der beschriebenen Rötung einhergehend mit Juckreiz seit 3 Tagen sowie allgemeinem Unwohlsein, Rücken- und Knieschmerzen hätten den behandelnden Klinikarzt veranlassen müssen, die Differentialdiagnose Borreliose in seine weiteren diagnostischen und therapeutischen Überlegungen einzubeziehen. Daß dies nicht erfolgt ist, ist als Diagnose- und demzufolge auch als Behandlungsfehler zu werten.
Dieser Fehler führte zu einer Verzögerung der Diagnostik und antibiotische Therapie um etwa sechs Wochen. Die in diesem Zeitraum bestehenden Beschwerden und Beeinträchtigungen durch die Borreliose sind dem ärztlichen Fehler anzulasten. Die Behandlung der Borreliose im Stadium I ist in der Regel kurativ, in Einzelfällen persistieren unspezifische Allgemeinsymptome wie Müdigkeit und Arthalgien für einige Wochen. Echte Therapieversager sind sehr selten. Somit sei auch für diesen Fall davon auszugehen, daß nach rechtzeitigem Therapiebeginn mit hoher Wahrscheinlichkeit mit einem umgehenden Abklingen der Symptomatik zu rechnen gewesen wäre.
Excerpt
Auszug aus der Begründung zur Petition
Seronegativity in Lyme borreliosis: 103 Peer-Reviewed Studies (in cache)
Congenital Transmission of Lyme: 28 Peer-Reviewed Studies (in cache)
Hintergrund
["insurance companies strictly adhere to Infectious Diseases Society of America (IDSA) guidelines" (Quelle),
While years of reviews have yet to result in any charges for treating Lyme according to these Guidelines, the Department of Health persists in targeting the ILADS doctors for a "review" that is intrusive, stressful, and exceedingly expensive to manage.
Nearly every ILADS doctor in New York who treats Lyme patients either is currently, or has been, under investigation. This is a political strategy being employed by powerful competitive interests who have been successful in influencing the State's Health Department's policies. New York is not the only state that has this problem, but it is one of the most egregious. Nationally, the situation has become so onerous that seven states have already enacted "Doctor Protection" legislation to prevent the targeting of ILADS doctors by medical review boards. New York has not enacted any such protections for our ILADS doctors.
Every doctor who finds himself in the crosshairs of the OPMC's review process must retain a highly specialized legal defense team to deal with the mountain of work that comes with these "reviews". For many of the doctors who have already been through this process, the legal bills have exceeded $50,000, and in some cases, even $100,000 or more.
The invariability of this expensive harassment has had a chilling effect on the involvement of any new practitioners who might want to get involved with Lyme disease. Many doctors simply will not treat Lyme patients because of the threat of having to deal with OPMC reviews..."
The release of Under Our Skin, 2: Emergence has brought further attention to films related to Lyme disease. This is a list of some of the Lyme disease movies/videos. There are also many news video clips on Lyme disease. It is not a complete list, but a start. If anyone can expand onto this, feel free to do so.
Lymelife Lymelife 2009: Official Movie Trailer. This video is not available in Germany. Invisible Illness and Incommunicable Diseases, Emily Reach White at TEDxGreenville, TED Talks Lyme Disease a Silent Epidemic, produced by France 5 Public Network and Grand Angle, directed by Chantal Perrin Maladie de Lyme diffusé sur France 5 le 20/5/14 (in French) The Voices of Lyme Disease- Breaking the Silence, created by Victoria Wilcox, a 16 year old girl and her friend, Sara Lynch. Youtube: "This video is not available. Sorry about that." Invisibly Ill, Documentary Film on Lyme Disease and Stealth Infections, Australia, feature length film Lyme disease? Bah! The Very Idea!, great Lyme Disease parody Ode to Lyme Brain [Forgetfulness] Lyme Awareness Video, OneTrueMedia.com
Celebrity Videos Yolanda Foster's Experience With Lyme: LRA Gala Daryl Hall Speaks About Persistent Lyme Disease Infection Dorothy Leland shared this story Debbie Gibson Reveals Drastic Weight Loss Caused by Lyme Disease Ben Stiller on David Letterman discusses Lyme disease Multiple Celebrities with Lyme Disease
Scientific Mason Kuhn, Lyme and Autism, video is half way down this blog Pr Luc Montagnier on Lyme disease, autism and chronic infections Lyme Disease - Seasons On The Fly, Dr Jason West
Political Rep. Scavello Asks About Lyme Disease at Health Budget Hearing, House Appropriations Committee, Department of Health.
Some ILADS videos http://www.ilads.org/lyme/lyme-videos.php http://www.ilads.org/lyme_programs/conference-videos.php http://ilads.org/ilads_media/boston-videos-home/ http://www.ilads.org/media/conference_land.php
Other 200 Videos about Lyme disease
Also, do an Internet search of
to find many additional videos.
Galbe JL, Guy E, Zapatero JM, Peerschke EI, Benach JL., Vascular clearance of Borrelia burgdorferi in rats.
Microb Pathog. 1993 Mar;14(3):187-201.
Wormser GP, McKenna D, Carlin J, Nadelman RB, Cavaliere LF, Holmgren D, Byrne DW, Nowakowski J. (fri PDF)
Brief communication: hematogenous dissemination in early Lyme disease.
Ann Intern Med. 2005 May 3;142(9):751-5. Summary for patients in: Ann Intern Med. 2005 May 3;142(9):I48.
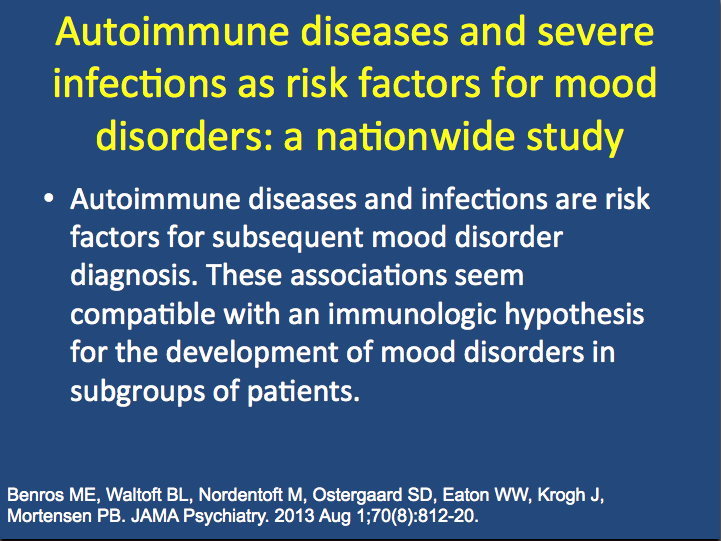
Progressive inflammatory reactions have been proposed as a model to explain disease progression in
Autism spectrum disorders associated with Lyme/tick-borne diseases may be mediated by a combination of inflammatory and molecular mimicry mechanisms.
Greater interaction is needed between infectious disease specialists, immunologists and psychiatrists to benefit from this awareness and to further understand these mechanisms.
Bransfield RC, Relationship of Inflammation and Autoimmunity to Psychiatric Sequelae in Lyme Disease. Psychiatric Annals. September 2012 - Volume 42, Issue 9: 337-341.DOI: 10.3928/00485713-20120906-07.
Prolonged inflammation, particularly the type associated with chronic infection within the CNS, is associated with further cognitive impairments, more severe psychiatric symptoms, gliosis, and dementia. Autoimmune effects also can be present at the same time and can include antineuronal antibodies and B. burgdorferilipoproteins that can disseminate from the periphery to inflame the brain.
These immune reactions can result in psychiatric symptoms such as obsessiveness, movement disorders, paranoia, and others. Autism spectrum disorders associated with Lyme disease and other tick-borne diseases appear mediated by a combination of inflammatory and autoimmune mechanisms from the mother's and/or infant's immune system. Understanding this pathophysiology will help physicians create new treatment options.
"Bildgebende Verfahren wie die SPECT (Einzelphotonen-Emissionscomputertomographie; aus dem Englischen: single photon emission computed tomography) können durch Messung der Perfusion Hinweise auf metabolische Veränderungen geben. Die SPECT erlaubt, die Perfusion einzelner Bereiche des Gehirns darzustellen. ... Alle 183 untersuchten Individuen erfüllten laut Autoren die Kriterien einer chronischen Lyme Borreliose. Perfusionsstörungen, vor allem im Frontal-, Schläfen- und Scheitellappen, wurden bei 75% der Patienten gefunden, bei seropositiven Patienten ebenso wie bei seronegativen Patienten. Verbesserungen oder komplette Normalisierung der Perfusion wurde bei 70% der behandelten Patienten nach mindestens 3 monatiger Gabe vor allem intrazellulär wirkender Antibiotika in einem Zeitraum von 1 bis 2 Jahren gesehen. Abnormalitäten im SPECT Scan, so die Autoren, werden bei der Mehrheit der Patienten/Innen mit chronischer Borreliose gesehen.
Die Aussage in der Arbeit wird wesentlich geschwächt, da keine Kontrollgruppe(n) untersucht wurde(n). So bleibt unklar, bei wie vielen Probanden im vergleichbaren Alters- und Geschlechterverhältnis (mit vergleichbarem Genussmittelkonsum und vergleichbarer Medikation) möglicherweise auch Auffälligkeiten/Abnormalitäten in der SPECT zu Tage treten. ... Ohne wohlausgewählte Vergleichsgruppen bleiben die Befunde leider weder objektiv noch beweisend. So könnten die Perfusionsstörungen durchaus Ausdruck anderer Störungen sein, die auf ganz andere Ursachen zurückgehen." (Quelle: DBG-Mitteilungen 2013-2, Seite 6)
Momentan existieren bei der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften nur zwei S1-Leitlinien, nämlich "Kutane Manifestationen der Lyme-Borreliose" und "Neuroborreliose". Hinzu kommt die Leitlinie "Diagnostik und Therapie der Lyme-Borreliose" der Deutschen Borreliose-Gesellschaft.
2. Healthcare providers need to be aware that currently published recommendations and
guidelines regarding treatment of Lyme disease are based on limited data. For example,
the recommendation that one does not need treatment for a tick bite if the tick has not
been imbedded for more than 48 hours was not based on testing in humans. Patients need
to be counseled to be aware of what are often only subjective symptoms (fatigue, aches
and pains, 'brain fog') that may occur several weeks to a few months after having been
bitten by a deer tick (Ixodes). It should be noted that these symptoms may be
inappropriately dismissed, or mischaracterized as psychiatric or stress-related. Guidelines
for antibiotic prophylaxis16 are also based on limited data. The recommendation that a
single day's treatment with doxycycline for an imbedded deer tick bite can prevent Lyme
disease has some published support; however, this approach may not always be effective,
and some physicians believe that it is ill-advised. Patients who have taken a prophylactic
dose need to be counseled to be aware that if symptoms develop over the subsequent few
months, they should seek medical attention. They should be made aware that antibody
production may be abrogated as a result of early dosing, thus potentially making
laboratory testing even more problematic in these situations.
3. Healthcare providers need also to be made aware that the recommendations regarding
antibiotic treatment of patients with persisting or relapsing symptoms are based primarily
on the results of one clinical trial. There have been a few other controlled treatment trials,
which did not show either any, or any sustained, benefit following treatment. But the
failure of the antibiotics used in these trials cannot be used to conclude that use of
different antibiotic regimens and durations of treatment would not be effective; there is
published information, in addition to physician experience, that suggest there are other
antibiotic regimens that may be effective. Until there are additional controlled treatment
trials to prove or disprove other antibiotic regimens, healthcare providers should make
themselves aware of available alternative regimens so that their patients can be provided
the opportunity to resolve their persisting symptoms.
4. Physicians should also be reminded of the Physician Protection Act17, which protects
them from any disciplinary action should they choose to diagnose and treat according to
clinical criteria, relying on history and symptoms even in the absence of positive lab
results. This may include prescribing antibiotics over a prolonged period of time when
warranted by the patient's presentation.
Lager A glaubt, dass die nach der Therapie weiter bestehenden Symptome auto-immun verursacht seien. Die Patienten erhalten nach 21 Tagen meist Antidepressiva und Schmerzmittel und werden nur noch symptomatisch behandelt, mit entsprechend geringer Wirkung. Der Haken an der Sache: Für diese "Auto-Immun-Hypothese" gibt es bis heute keinen Nachweis!
Lager B nimmt an, dass die persistierenden Symptome dieser Patienten durch eine noch nicht ausgeheilte Borreliose verursacht werden. Sie lassen den Patienten die Wahl, auch im Sinne der in Deutschland geförderten, partizipativen Entscheidungsfindung (3), eine erneute oder verlängerte antibiotische Behandlung zu versuchen. Diese Ärzte machen die Therapiedauer von der individuellen Vorgeschichte (u. a. Immunstatus, Vorerkrankungen, Co-Infektionen) und dem Ansprechen des Patienten auf die Therapie abhängig.
Bei der Borreliose im fortgeschrittenen Stadium verliert sich der Grund, warum die Patienten nach der Standardtherapie immer noch leiden, im Nebel nicht-bewiesener Hypothesen. Für eine persistierende Infektion sprechen inzwischen allerdings neue Forschungsergebnisse (4)...
Falls auch Sie Ihren Namen unter diesen offenen Brief setzen möchten, schreiben Sie bitte eine kurze Mail (die Namen reichen) mit dem Betreff “Offener Brief” an:
Literatur zum Offenen Brief, Januar 2013.
[Eine umfangreiche Zusammenstellung von Arbeiten zu
When quantitative effects on biofilm-like colonies were evaluated,
In this study, we investigated the hypothesis that these aggregates are
indeed biofilms, structures whose resistance to unfavorable conditions are well documented. Biofilm
formation by Borrelia species might play an important role in their survival in diverse environmental conditions by providing
refuge to individual cells.
We studied Borrelia burgdorferi
for several known hallmark features of biofilm, including
using several modes of microscopic, cell and molecular biology techniques.
In
summary, we have found substantial evidence that Borrelia burgdorferi is capable of forming biofilm in vitro.
"Therapie der Borreliose, insbesondere der chronischen Neuroborreliose, aus Sicht der neurolog. Rehabilitationsmedizin, des Akut-Krankenhauses und unter speziellen neurochirurgischen Aspekten",
Anmeldung bei Gert Schlegel, Borreliose-SHG Leipzig, Hans-Marchwitza-Str. 28, 04279 Leipzig, Tel. (0341) 338-2155
Frage: Wenn man einen Zeckenstich an seinem Körper entdeckt, was sollte man dann tun?
Dr. Burgdorfer: Ein Arzt sollte konsultiert werden und er sollte sofort mit einer Antibiotika-Behandlung beginnen. Vor allem wenn eine Wanderröte, also ein roter Fleck um die Einstichstelle herum, entdeckt wird.
Eleanor D. Hynote, Phyllis C. Mervine, Raphael B. Stricker, "Clinical evidence for rapid transmission of Lyme disease following a tickbite", Diagn Microbiol Infect Dis. 2011 Nov 18.
We describe 3 cases in which transmission of Borrelia burgdorferi appears to have occurred in less than 24 h based on
The animal transmission studies have several significant limitations, however:
Our data indicate that topical treatment with a formulation containing azithromycin is a promising approach to prevent Lyme borreliosis shortly after a tick bite.
"Chronically ill patients with neurodegenerative, neurobehavioural and psychiatric diseases commonly have systemic and central nervous system bacterial and viral infections. In addition, other chronic illnesses where neurological manifestations are routinely found, such as fatiguing and autoimmune diseases, Lyme disease and Gulf War illnesses, also show systemic bacterial and viral infections that could be important in disease inception, progression or increasing the types/severities of signs and symptoms."
Garth L. Nicolson, J. Haier, Role of Chronic Bacterial and Viral Infections in Neurodegenerative, Neurobehavioral, Psychiatric, Autoimmune and Fatiguing Illnesses:
Antikörper, die an rekombinante Antigene binden, weisen
einen hohen Grad an Selektivität auf. Man geht aber auch bei
diesen Antikörpern von unspezifischen Bindungen aus,
sodass der Cut [d.h. die Trennung zwischen test-positiv und test-negativ] vom Hersteller jeweils angepasst wird. Die
analytische Sensitivität ist hierbei ungewiss [d.h. wieviele von den tatsächlich Kranken erkannt werden]. Dies ist auch
bedingt durch die Vielfalt an pathogenen Stämmen, die nicht
sicher von einzelnen Antigenen erfasst werden.
Antikörper ("Y") und Antigene
LB und Alzheimer/ Interview Dr. MacDonald (ILADS-Arzt).
Vor allem der Fall eines Feuerwehrmannes, Paul Christensen, brachte ihn viel weiter. Dr. MacDonald konnte zeigen, dass die Hirnareale mit Alzheimer-ähnlichem Schaden die gleichen waren wie die Areale mit Spirochäten-DNA. Er benutzte dazu fluoriszierend gefärbtes Bb-DNA.
Er betont die Ähnlichkeit mit dem Syphilis-Erreger und das Vorkommen der Sonderformen , die leicht übersehen würden. Ebenso die Biofilme, die schon im Film "Under our Skin" erwähnt wurden. Im Biofilm d.h. in der Bb-Kolonie seien eher die Sonderformen vorhanden, was diese Kolonien ziemlich AB-resistent mache, vor allem wegen einer gel-artigen Schutzschicht . Er erwähnt auch noch mal die Möglichkeit der vertikalen Infizierung von Mutter auf Kind durch die Plazenta. (Siehe frühere Artikel im Internet, auch im Buch Hans Horst). Auch dass LB lange Zeit eine latente/ruhende Infektion sein könne, oder dass Patienten bei Schwächung des Abwehrsystems aus irgendwelchen Gründen noch nach zwanzig oder dreißig Jahren Spätsymptome entwickeln können (Reaktivierung -zB Bb-Herde in der Haut bei ACA; sich dadurch entwickelnder Gewebeschaden hieße immer noch eine aktive Infektion), Resultate, die medizinisch-politisch nicht gerne gehört werden...
FSME /RKI Zahlen 2009 nach Hinweis NGZ 6.5.2010: "Die Zahl der Hirnhautentzündungen durch Zeckenbisse hat vergangenes Jahr leicht zugenommen. In 2009 erkrankten in D 313 Menschen an....FSME und somit 8 % mehr.....wie das RKI in Berlin mitteilte...."
Kenntnis der Infektionsorte ist notwendig für die Präzisierung der Risikogebiete. Bei 300 Meldungen lag er in D. Die Zahl der Risikogebiete bleibt bei 136 bundesweit konstant und unverändert.
(Risikogebiet: deutlich mehr als 1 Fall auf 100.000 Einwohner innerhalb 5 Jahren.)
Die Inzidenz der FSME kann durch Steigerung der Impfrate reduziert werden, gäbe aber ein falsches Bild über das Risiko. Dann wären weitere Kriterien für die Risikoerfassung notwendig wie zB Zeckenvorkommen, Durchseuchung, Erfassung Impfquoten und Tierbefall, die es bisher nicht ausreichend gibt. Deshalb bastelt man an einen möglichen Korrekturfaktor.
Ältere Menschen scheinen sich weniger impfen zu lassen als die Kinder, hätten aber ein viel höheres Risiko nach Infektion ernsthaft zu erkranken.
Bei FSME-Verdacht: Eine frühere FSME-Impfung oder eine gegen Gelbfieber oder Japan-Enzephalitis oder ein durchgemachtes Denguefieber können die Diagnose fälschen; hier seien Verlauftests unverzichtbar.
Impf-Empfehlung: nur für Menschen, die a. in Risikogebieten wohnen/arbeiten und b. zeckenexponiert sind, inkl. beruflich Gefährdete da. Für diese Gruppen ist die Kostenerstattung der Kassen pflichtmäßig,
Eine Impfprophylaxe wird auch als sinnvoll gesehen bei Freizeit-Zeckenexponierung, auch da wo nur vereinzelte Fälle auftraten. Ebenso für Reisende in Endemiegebiete außer Deutschland.
Mit PCR wurde die Durchseuchung ermittelt. Bartonella und Mykoplasmen wurden hierbei nicht berücksichtigt:
Man erwartet weitere die Enddaten gegen Ende 2009. Verbreitungs-Karte der Teilnehmer und Statistik
"In der deutschsprachigen medizinischen Literatur wird die Krankheit "Chronische Borreliose" noch gerne negiert bzw. als nicht heilbares "Post Lyme Syndrom" bezeichnet. Die dahinter stehende wissenschaftliche Meinung vertritt die Auffassung, dass die Borrelien durch eine Behandlung mit Antibiotika über 2-3 Wochen vollständig vernichtet werden. Sollten danach noch Beschwerden auftreten, so resultieren diese nicht von den Borrelien sondern z.B. von noch weiter wirkenden chronischen Entzündungen.
Diese Auffassung wird vom BCA und der Deutschen Borreliose-Gesellschaft nicht geteilt. Sie berufen sich in diesem Zusammenhang auf umfangreiche Studien der ILADS sowie eigene Erkenntnisse und Erfahrungen. Danach sind Borrelien recht "intelligente", fortbewegungsfähige Spiralbakterien, die es recht gut verstehen, sich der körpereigenen Immunabwehr als auch bestimmten Antibiotika zu entziehen. Evtl. haben Sie bereits davon gehört, dass Borrelien "persistieren", d.h. sich "tarnen" und "verstecken" können.
Die in der Deutschen Borreliose-Gesellschaft e.V. organisierten Ärzte und das BCA setzen auf eine Langzeitantibiose über mehrere Monate, evtl. auch mit wechselnden Präparaten. Diese Ärzte haben Erfahrung mit dem breiten Spektrum der Antibiotika und empfehlen Begleitmaßnahmen, um mögliche Nebenwirkungen der Antibiotika von Anfang an so weit als möglich zu kompensieren.
Die wissenschaftliche Unterlegung der vom BCA vertretenen Diagnostik- und Therapie-Konzepte stützt sich u.a. auf folgende Publikationen:
Bücher/Dokumente:
Mitgliederversammlung der Deutschen Borreliose-Gesellschaft am 20. März 2009, 16:40 Uhr, in Tabarz zwischen Eisenach und Gotha. Auf der Tagesordnung steht eine Satzungsänderung (Vortragsprogramm)
Pauliina Hartiala, Immune evasion by Borrelia burgdorferi������������������ with special reference to CD38 mediated chemotaxis of neutrophils and dentritic cells, Department of Medical Microbiology and Immunology, University of Turku and Turku Postgraduate School of Biomedical Sciences, Turku, Finland (Matti K. Viljanen, MD, supervisor)
Dr. Petra Hopf-Seidel ist seit 1980 Ärztin. Sie lebte 3 Jahre in Malaysia, wo sie sich u. a. mit ganzheitlicher Therapie beschäftigte. Nach der Ausbildung zur Allgemeinmedizinerin schloss sie eine Ausbildung zur Fachärztin für Neurologie und Psychiatrie an und erwarb die Zusatzbezeichnung "Chirotherapie". Seit 2005 arbeitet sie in ihrer Privatpraxis für Neurologie und Psychiatrie in Ansbach.
Emir Hodzic (Real-Time PCR Research and Diagnostic Core Facility, School of Veterinary Medicine, University of California at Davis, California, United States of America)
Lyme Borreliosis: is there a preexisting (natural) variation in antimicrobial susceptibility among
Borrelia burgdorferi
strains?
Informationen von Günter Schust
... An inspriring story detailing my struggle with Lyme disease and how after 18 years, against the odds I survived it.
... Eine inspirierende Geschichte, die einen Kampf mit der Lyme-Borreliose beschreibt und wie sie nach 18 Jahren gegen alle Widrigkeiten überlebt wurde.
Solche Fälle gibt es sehr viele im Verborgenen (Buch: "Die verschwiegene Epidemie" von Birgit Jürschik Busbach), und ich bekomme noch immer Anrufe von verzweifelten Menschen, die keine adäquate Therapie bekommen. Ich kenne einige Suizidfälle mir persnlich bekannter Borreliosekranker. Erst vor ein paar Monaten hat wieder ein mir gut Bekannter aus Verzweiflung und Aussichtslosigkeit sein Leben auf dem Bahngleis beendet. Und wenn es so weit kommt, dass ein Arzt sein Vermögen verliert, weil er aus Berufung seine Patienten optimal versorgt, in Regress genommen wird, wegen mehrfacher Budgetüberziehung, dann ist das ein unglaublicher Skandal.
Informationen von Corry Welker
Bericht 18. März 2019
Edition One: The Ad Hoc Committee for Health Equity in ICD11 Borreliosis Codes
(Bericht an UNO und USA Congress über die Situation der Lyme-Borreliose Patienten, deutsche Übersetzung von Teilen von Ursula Talib-Benz)
... [P]oor healthcare response is not happening because better methods of diagnosis and treatment do not exist - in fact they do. It is happening because of corruption, conflicts of interest and unethical practices that are ignored or even promoted by State Actors, their agents and vested business interests ["institutional corruption"]. This report will show how conflicts of interest, market competition, State Actor collusion with private sector profiteers and other nonmedical and non-science-based dynamics are destroying the capacity to provide care for estimated millions living with Lyme ...
Uta Everth, Leitlinienstandards -
Am Beispiel der S3 Leitlinie zur Neuroborreliose, Erörterung zur Leitlinie Neuroborreliose der Deutschen Gesellschaft für Neurologie (DGN)
Das Europäische Parlament setzt sich intensiv mit Fragen und Diskrepanzen um LB auseinander. Die nächste Sitzung ist noch diesen Januar. Die vorläufig angenommenen Punkte.
CC: Jens Spahn, Bundesminister für Gesundheit
Von: Günther Schust
Datum: 11. Dezember 2018
bereits vor einiger Zeit habe ich erfahren, dass man dem Borreliose-behandelnden Arzt Herrn Hans-Peter Gabel in Wolfenbüttel wegen Budget-Überschreitung in Regress genommen und ihm damit sein gesamtes privates Vermögen liquidiert hat. Seine Kassenärztliche Zulassungen hatte man ihm belassen, damit er weiterhin seine Borreliose-kranken Kassenpatienten behandeln kann.
Jetzt erfahre ich, dass Sie Herrn Gabel auch noch die Kassenzulassung entzogen haben und damit auch noch seine berufliche Existenz liquidieren. Das kann ich mit großer Entrüstung kaum fassen. Herrn Gabel kenne ich persönlich aus der Deutschen Borreliose-Gesellschaft als sehr engagierten Arzt, der sich in ungewöhnlicher Weise mit viel persönlichem Einsatz erfolgreich für seine meist schwerkranken Patienten für deren Genesung einbringt. (weiterlesen)
Von: Günther Schust
Datum: 31. Januar 2019
(Datum: 22. Januar 2019)
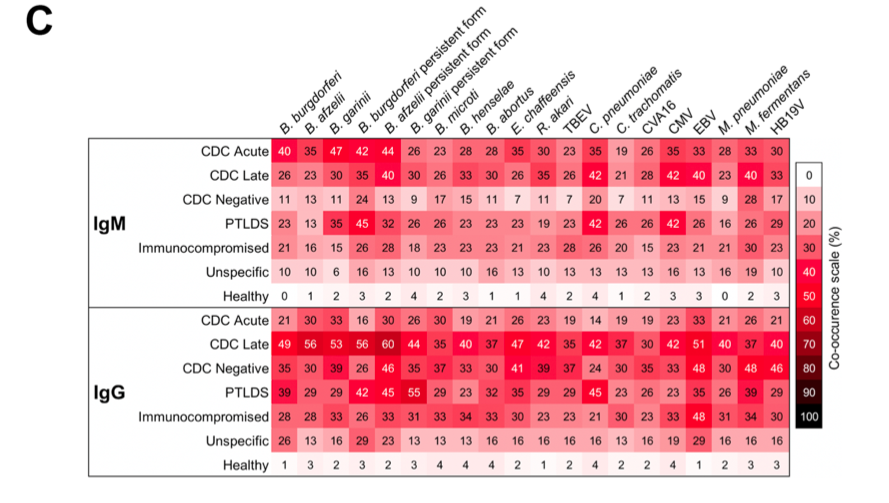
Quelle der Abbildung: Fig. 2 C in Evaluating polymicrobial immune responses ...
IgM and IgG responses by individual patient categories to 20 microbes. Patients are classified according to the Centers for Disease Control and Prevention (CDC) and other categories
Example 1: CDC Acute individuals: 40% of them have B burgdorferi, 35% have B. afzelii, 47% have B. garinii etc.
Example 2: Healthy individuals: 0% of them have B burgdorferi, 1% have B. afzelii, 2% have B. garinii etc.
weisen darauf hin, dass man bei chronisch/langwierig Erkrankten nach Zechenstich viel breiter nachschauen müsse als nur nach Borrelia burgdorferi.
2 Department of Biology and Environmental Science, University of New Haven, West Haven, CT 06516, USA; ten.ipasave@hnu (E.S.); moc.liamg@hsulif.r.enirehtak (K.R.F.)
3 Australian Biologics, Sydney, NSW 2000, Australia; ua.moc.scigoloibnailartsua@ekrub.einneJ
4 School of Health Sciences, Universidad Catolica Santiago de Guayaquil, Guayaquil 090615, Ecuador; ua.moc.tensutpo@ocnarf.nitsuga
5 Union Square Medical Associates, 450 Sutter Street, Suite 1504, San Francisco, CA 94108, USA; moc.liamg@relsefcassilem
(Datum: 1. Juli 2018)
Connie Strasheim, New Paradigms in Lyme Disease Treatment: 10 Top Doctors Reveal Healing Strategies That Work, 2016
(Datum: 9. April 2018)
W. Berghoff, Klinische Grundlagen der antibiotischen Behandlung bei Borreliose, 2007 (im Cache)
... Das Erythema migrans tritt möglicherweise erst Wochen oder Monate nach Zeckenstich auf. In solchen Situationen ist es fraglich, ob das Erythema migrans hilft, den Zeitpunkt der Dissemination zu bestimmen. Zudem sei bereits an dieser Stelle erwähnt, dass auch nach "adäquat behandeltem Erythema migrans" eine Spätborreliose auftreten kann. Dies impliziert selbstverständlich, dass durch eine solche adäquate Behandlung des Erythema migrans die Dissemination nicht verhindert wurde oder zum Zeitpunkt der vermeintlich adäquaten antibiotischen Behandlung nicht mehr ein lokalisiertes, sondern bereits ein disseminiertes Frühstadium vorlag.
(Datum: 4. März 2018)
Patient Centered Care Advocacy Group, May 19, 2016, 07:00 ET
WASHINGTON, May 19, 2016 /PRNewswire/ -- The examination of autopsied brain tissues from patients who died of serious neurological conditions has revealed that many tick-borne infections, such as Lyme disease, go undiagnosed and untreated. Board-certified pathologist, Alan B. MacDonald, MD, says his research shows "tick infections are not easily detected with routine tests, nor are they easily cured with short courses of antibiotics."
2. Alan B. MacDonald, Nematode filarial Worms in Cerebrospinal Fluid of a Multiple Sclerosis Patient at Autopsy,
F1000 Research, 19 January 2016, doi.org/10.7490/f1000research.1111264.1
(im Cache)
Abstract:
Multiple Sclerosis is classified according to current nosology as a human neurodegenerative [demyelinating] disorder, which is favored to be an autoimmune process. The actual causation of Multiple Sclerosis has not been agreed upon. Loss of myelin in the brain and spinal cord tissues is accompanied by diverse additional microscopic abnormalities in the plaques of MS. Subsequent investigation raised the possibility of chronic deep brain and spinal cord spirochetal infections {Steiner, Ichelson, Marshall and others} as the de facto cause of mylein loss in Multiple Sclerosis.
WEBWIRE, Washington, DC, May 19, 2016 (im Cache)
The examination of autopsied brain tissues from patients who died of serious neurological conditions has revealed that many tick-borne infections, such as Lyme disease, go undiagnosed and untreated. Board-certified pathologist, Alan B. MacDonald, MD, says his research shows "tick infections are not easily detected with routine tests, nor are they easily cured with short courses of antibiotics". ... MacDonald found two Borrelia pathogens, including B. burgdorferi the causative agent of Lyme disease, thriving inside parasitic nematode worms, worm eggs or larvae in the brain tissue of nineteen deceased patients. These microscopic worms are endosymbionts, meaning the Borrelia bacteria dwell inside the worms. A tick bite delivers the nematode into the human body.
London (England) Lecture, May 15, 2016, Lyme Disease Science and Policy Challenges Forum, Washington, DC, May 19, 2016 (hosted by the Lyme Action Network)
Spirochetes reside inside of the nematodes (endosymbiont borrelia). Endosymbiont released after the death of the nematode. Migrating worm destroys myelin in the brain. Hundreds of brain specimen slides studied to find one worm. It is much easier to find worms in csf.
10 patients with Multiple Sclerosis - 10 spinal fluids contain nematode adults, larval forms and eggs.
(Datum: 14. Dezember 2017)
Alison W. Rebman1, Kathleen T. Bechtold2, Ting Yang1, Erica A. Mihm1, Mark J. Soloski1, Cheryl B. Novak1 and John N. Aucott1* (1 Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 2 Department of Physical Medicine and Rehabilitation, Johns Hopkins University School of Medicine, Baltimore, MD, United States), The Clinical, Symptom, and Quality-of-Life Characterization of a Well-Defined Group of Patients with Posttreatment Lyme Disease Syndrome, Front. Med., 14 December 2017
Conclusion: Although physical exam and clinical laboratory tests showed few objective abnormalities, standardized symptom questionnaires revealed that patients with PTLDS are highly and clinically significantly symptomatic, with poor health-related quality of life. PTLDS patients exhibited levels of fatigue, musculoskeletal pain, sleep disturbance, and depression which were both clinically relevant and statistically significantly higher than controls. Our study shows that PTLDS can be successfully identified using a systematic approach to diagnosis and symptom measurement. As the prevalence of PTLDS continues to rise, there will be an increased need for physician education to more effectively identify and manage PTLDS as part of integrated patient care.
(Datum: 25. November 2017)
Corry Welker, Rundmail 64 (13. November 2017) mit Anhängen
(Datum: 20. April 2017)
Nachricht von Günther Schust, 20. April 2017
(Datum: 5. März 2017)
Sue Ferrara, Lyme Bacteria Hides Inside Parasitic Worms, Causing Chronic Brain Diseases, May 19, 2016 (im Cache).
Recent discovery confirmed by state-of-the-art Molecular Beacon DNA probes
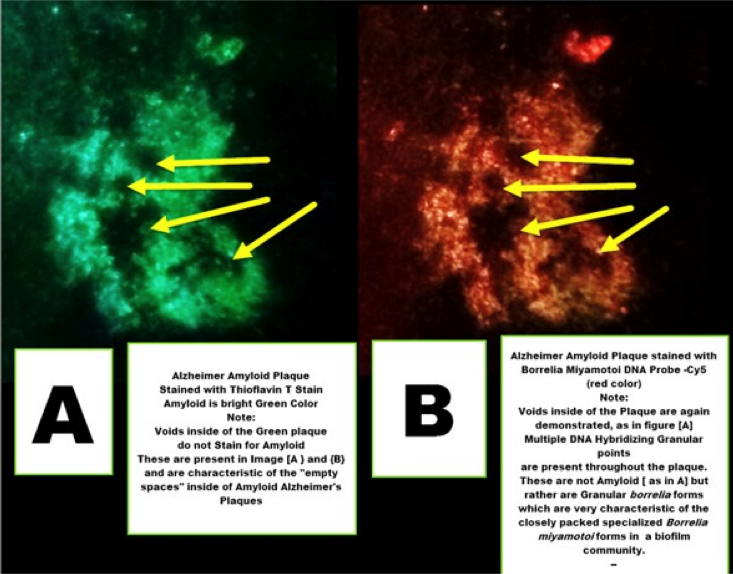
An Alzheimer plaque stains equally for beta-amyloid and Borrelia DNA. Many researchers now believe that the amyloid is not a cause of dementia, but an anti-microbial peptide defending the body by coating the infecting organisms.
Quelle: Dr. Paul Duray Research Fellowship Endowment Inc.
Alan MacDonald, Borrelia Dwells in Parasitic Nematodes in Glioma & Neurodegenerative Disease (im Cache)
For decades our public health agencies have insisted that current antibody testing and short courses of antibiotics for Lyme disease are adequate.
This view now needs to be discarded.
(Datum: 11. Februar 2017)
Emily R. Adrion, John Aucott , Klaus W. Lemke, Jonathan P. Weiner, Health Care Costs, Utilization and Patterns of Care following Lyme Disease, Public Library of Science PLoS ONE 10(2): e0116767, February 4, 2015. http://dx.doi.org/10.1371/journal.pone.0116767
deutsche Zusammenfassung: Analyse der Johns-Hopkins-Studie zum Thema Behandlungskosten von Borreliose-Patienten nach initialer Antibiotikatherapie, Borreliose-Nachrichten, 18. März 2016.
Approximately 10 - 20% of patients treated for Lyme disease with a recommended 2 - 4 week course of antibiotics will have patient-reported symptoms that may last for weeks, months or years. [7] [8] Post-treatment Lyme disease symptoms have been described by numerous investigators and include fatigue, musculoskeletal pain, and neurocognitive complaints such as poor memory and concentration and extremity dysthesias. In some cases, symptoms may be severe, chronic and adversely affect health-related function. [8] [9] [10] [11] When post-treatment Lyme disease symptoms (PTLDS) persist for six months or longer and are associated with functional limitations in the patient, the illness has been termed "Post-treatment Lyme Disease Syndrome" by the Centers for Disease Control. [7] Because no sensitive biomarker for remotely treated Lyme disease exists, the true number of individuals at risk for the syndrome is unknown. [12] [13]
Welcher Zusammenhang besteht zwischen der Lyme-Borreliose und dem Post-Treatment Lyme Disease Syndrome (PTLDS), und mit welcher Wahrscheinlichkeit kommt es zur Entwicklung von PTLDS?
Welche finanziellen Belastungen entstehen im amerikanischen Gesundheitswesen durch das Post-Lyme-Syndrom?
(Datum: 11. August 2016)
Corry Welker, Rundmail 62 (35 Seiten, 7. Februar 2016)
darin unter anderem:
Another limitation of our study is that it was not directed at patients with extracutaneous manifestations of Lyme disease. Data from certain European studies have suggested that impairment in health-related quality of life may occur as a consequence of neurologic Lyme disease specifically [9, 11].

(Datum: 21. Dezember 2015)
Alexandra Vogl, Borreliose - Warum Anzeichen meist schwer zu erkennen sind
(Datum: 4. Dezember 2015)
Elsner RA, Hastey CJ and Baumgarth N, CD4+ T Cells Promote Antibody Production but Not Sustained Affinity Maturation during Borrelia burgdorferi Infection,
Infect Immun. 2015 Jan;83(1):48-56. doi: 10.1128/IAI.02471-14. Epub 2014 Oct 13
CD4 T cells are crucial for enhancing B cell-mediated immunity, supporting the induction of high-affinity, class-switched antibody responses, long-lived plasma cells, and memory B cells [humoral response]. Previous studies showed that the immune response to Borrelia burgdorferi appears to lack robust T-dependent B cell responses, as neither long-lived plasma cells nor memory B cells form for months after infection, and nonswitched IgM antibodies are produced continuously during this chronic disease. ...
For immune systems basics see
Hastey CJ, Elsner RA, Barthold SW, Baumgarth N, Delays and Diversions Mark the Development of B Cell Responses to Borrelia burgdorferi Infection, J Immunol. 2012 Jun 1;188(11):5612-22. doi: 10.4049/jimmunol.1103735. Epub 2012 Apr 30.
B cell responses modulate disease during infection with Borrelia burgdorferi, the causative agent of Lyme disease, but are unable to clear the infection.
Overall, the study indicates that B. burgdorferi might evade B cell immunity by interfering with its response kinetics and quality.
(Datum: 20. Juli 2015)
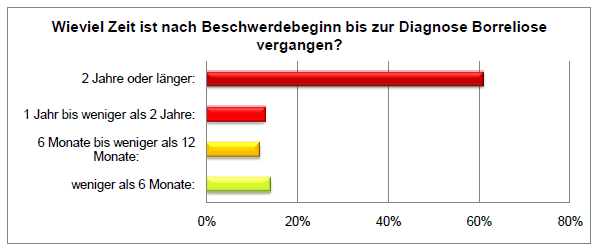
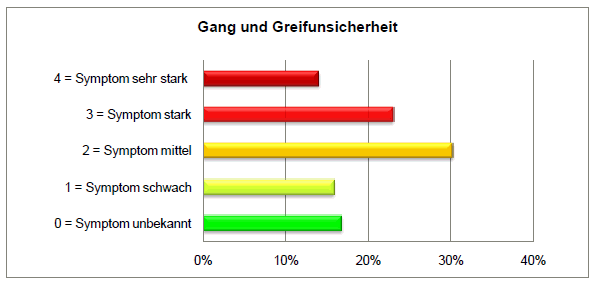
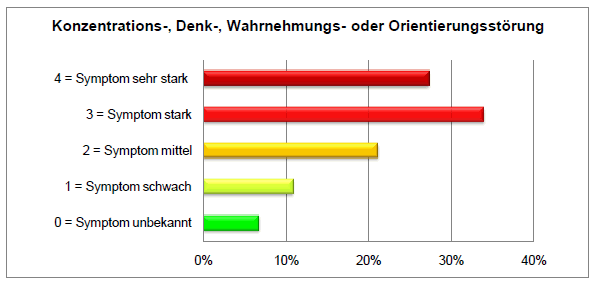
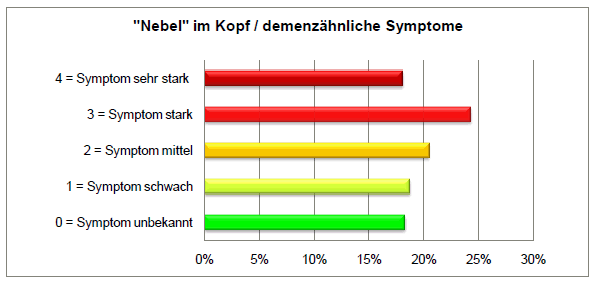
Borreliose-Nachrichten, Auswertung unserer Umfrage unter Betroffenen, Stand: 14.7.2015
(Datum: 13. Juli 2015)
Michael J Cook, Lyme borreliosis: a review of data on transmission time after tick attachment, Int J Gen Med. 2015; 8: 1 - 8. Published online 2014 Dec 19. doi: 10.2147/IJGM.S73791, PMCID: PMC4278789

click on figure to enlarge
Source
Conclusion:
"The claims that removal of ticks within 24 hours or 48 hours of attachment will effectively prevent LB are not supported by the published data, and the minimum tick attachment time for transmission of LB in humans has never been established.
(Datum: 19. Mai 2015)
Angela Senders, Helané Wahbeh, Rebecca Spain, and Lynne Shinto, "Mind-Body Medicine for Multiple Sclerosis: A Systematic Review", Autoimmune Diseases Volume 2012 (2012), Article ID 567324, 12 pages
The objective of this paper was to assess the published evidence for using mind-body techniques for symptom management of multiple sclerosis. 4 high quality studies showed that
Study
Intervention
Helpful for
Ghafari et al. 2009
Relaxation
Quality of Life
Grossmann et al. 2010
Mindfulness-based stress reduction
Depression
Anxiety
Fatigue
Quality of Life
Oken et al. 2004
Yoga
Fatigue
McClurg et al. 2006
Biofeefback
Bladder Incontinence
The remaining studies demonstrated benefit for balance and daily pain intensity, but had no effect on executive function, mood, or disability -although many methodological inadequacies were identified.
S. Ghafari, F. Ahmadi, M. Nabavi, K. Anoshirvan, R. Memarian, and M. Rafatbakhsh, "Effectiveness of applying progressive muscle relaxation technique on quality of life of patients with multiple sclerosis," Journal of Clinical Nursing, vol. 18, no. 15, pp. 2171-2179, 2009.
(Datum: 28. April 2015)
Lyme Connection, "Meet the Lyme Disease Experts: Dr. Richard Horowitz" (medical director, Hudson Valley Healing Arts Center), 2015 (in cache).
"People who come to see me who have chronic Lyme disease usually have multiple overlapping factors keeping them ill. I've labeled this Lyme-MSIDS: Multiple Systemic Infectious Disease Syndrome. MSIDS is a 16-point model.
and many patients have several of these infections simultaneously, keeping them ill.
Then you've got viral infections showing up in ticks, like the
We don't see these viruses a lot, but we do occasionally see a reactivation of other viruses like EBV, CMV and HHV-6.
All of these illnesses can be caused by Lyme, which is known as the "great imitator". The questionnaire would reveal whether we are dealing with a multi-systemic illness, which is classic for Lyme disease. Then you add up the four sections of the questionnaire, and if their score is over 46, there's statistically a good chance that they suffer from Lyme disease.
(Datum: 25. April 2015)
Cameron D, Relying on a Negative Lyme Disease Test Can Prove Deadly, Daniel Cameron, April 21, 2015.
"... a paper published in the March issue of Cardiovascular Pathology, reports the adolescent, in fact, had died from Lyme carditis. [Esther C. Yoon, Eric Vail, George Kleinman, Patrick A. Lento, Simon Li, Guiqing Wang, Ronald Limberger, John T. Fallon, Lyme disease: a case report of a 17-year-old male with fatal Lyme carditis, March 21, 2015]
(Datum: 25. April 2015)
Molins CR1, Ashton LV2, Wormser GP3, Hess AM4, Delorey MJ1, Mahapatra S2, Schriefer ME1, Belisle JT2.
[1 = Division of Vector-Borne Diseases, Centers for Disease Control and Prevention,
2 = Department of Microbiology, Immunology, and Pathology, Colorado State University, Fort Collins,
3 = Department of Medicine, Division of Infectious Diseases, New York Medical College, Valhalla, New York,
4 = Department of Statistics, Colorado State University, Fort Collins],
Background: Early Lyme disease patients often present to the clinic prior to developing a detectable antibody response to Borrelia burgdorferi, the etiologic agent. Thus, existing 2-tier serology-based assays yield low sensitivities (29%-40%) for early infection. The lack of an accurate laboratory test for early Lyme disease contributes to misconceptions about diagnosis and treatment, and underscores the need for new diagnostic approaches.
See also: New Approach to Diagnosing Lyme Disease Shows Promise, National Institute of Allergy and Infectious Diseases, April 17, 2015.
(Datum: 24. März 2015)
Corry Welker, Rundmail 60 (12 Seiten, 17. März 2014), 61 (30 Seiten, 4. März 2015)
Ein kleiner Auszug
The guidelines address three clinical questions
Healthcare providers who evaluate and manage patients with Lyme disease are the intended users of the new ILADS guidelines, which replace those issued in 2004 (Exp Rev Anti-infect Ther 2004;2:S1-13). These clinical practice guidelines are intended to assist clinicians by presenting evidence-based treatment recommendations, which follow the Grading of Recommendations Assessment, Development and Evaluation system.
Prohibits the investigation of any claim of medical professional misconduct based solely on treatment that is not universally accepted by the medical
profession.
This act requires the Vermont State Board of Medical Practice, the Vermont Board of
Osteopathic Physicians, the Office of Professional Regulation, and the Vermont Board of
Nursing to issue a policy statement to physicians, naturopathic physicians, and advanced
practice registered nurses, respectively. ... The policy statement must ... state that precluding errors, omissions, or other
unprofessional conduct, the respective Board or Office of Professional Regulation will
not pursue disciplinary action against a physician, naturopathic physician, or advanced
practice registered nurse solely for use of medical care recognized by the guidelines of
the Centers for Disease Control and Prevention, Infectious Diseases Society of America,
or International Lyme and Associated Diseases Society for the treatment of a patient's
Lyme disease or other tick-borne illness symptoms.
Seitens des verantwortlichen Klinikarztes wurde zu diesen Vorwürfen Stellung genommen. Bei Aufnahme sei eine korrekte Anamnese und klinische Befunderhebung vorgenommen worden. Von einem Insektenstich oder einer Zeckenbißverletzung sei nie die Rede gewesen. Auch seien in den Behandlungsunterlagen zweimal "keine Beschwerden" eingetragen worden. Klinische Hinweise auf eine Borreliose hätten seinerzeit nicht bestanden.
abzuleiten. Es sei sehr wahrscheinlich, daß die zu Beginn des Klinikaufenthaltes aufgetretene allgemeine Symptomatik in Verbindung mit dem dokumentierten Hautbefund der rechten Wade bereits der Borreliose entsprach. Allerdings sei fraglich, ob zu diesem Zeitpunkt bereits die Borreliosereaktionstests positiv gewesen wären.
(Datum: 20. November 2014)
Robert C. Bransfield, M.D., The Neuropsychiatric Lyme Assessment (in cache)
(Notation: * = highly diagnostic significance)
Can you sustain your attention upon significant events in your environment?
Can you prioritize and allocate your attention upon the most significant perceptions of your environment?
Do you easily lose your capacity for attention when frustrated?
Are you easily distracted from excessive sensitivity to any of the following: *Auditory - Visual - Tactile - Olfactory
(Datum: 14. November 2014)
change.org-Petition von Carl Tuttle, Calling for a Congressional investigation of the CDC, IDSA and ALDF
Carl Tuttle, 33 David Dr, Hudson, NH03051,
Website: New Hampshire Lyme Misdiagnosis
Carl Tuttle, Lyme disease antiscience, Letter to the Editor, The Lancet Infectious Diseases, Volume 12, Issue 5, Page 362, May 2012 (in cache)
The Tuttle family was featured on New Hampshire Chronicle's "Living with Lyme" with the program archived on their site in six segments (Part 1, Part 2, Part 3, Part 4, Part 5, Part 6)
Persistent Lyme infection: 273 Peer-Reviewed Studies (in cache)
After spending four years on this subject the following statement from a physician on the front lines treating the late stage Lyme epidemic for a quarter century rings true:
"In the fullness of time, the mainstream handling of chronic Lyme disease will be viewed as one of the most shameful episodes in the history of medicine because elements of academic medicine, elements of government and virtually the entire insurance industry have colluded to deny a disease."
We have studies proving persistent infection after antibiotic treatment for mice, dogs, ponies, monkeys, cows, iris biopsy, and ligamentous tissue but if you perform a simple Yahoo search for the following statement, "There is no convincing scientific evidence that chronic Lyme exists" you will find the top search results are connected to "elements of academic medicine" involved in the denial of the late stage Lyme epidemic.
Weitere Informationen in der Petition
(Datum: 6. November 2014)
Liste (als pdf) gegen Borrelien wirksamer Antibiotika und Antiprotozoika (zusammengestellt von Friedhelm Bausen, Stand Juni 2008)
(Datum: 11. Oktober 2014)
The New York State Department of Health Office of Professional Medical Conduct (OPMC) has closed the case of Dr. Kari W. Bovenzi (in cache) (Woman of Distinction 2013, New York State Senate) without further action anticipated. According to Jacques Simon, her attorney, this may set an important precedent that physicians will no longer be investigated or charges threatened or levied when the issue is solely extended antibiotic therapy for patients being treated for Lyme disease (or suspected Lyme disease).
Kari W. Bovenzi, "Why Lyme Doctors Need Defense Funds"
"It's an unfortunate fact of life these days that a group of physicians who treat tick-borne diseases in accordance with the authorized ILADS (International Lyme and Associated Diseases Society) Guidelines invariably come under "review" by the New York State Department of Health's Office of Professional Medical Conduct.
Kritik an den IDSA guidelines von der Deutschen Borreliose-Gesellschaft]
(Datum: 1. September 2014)
Robert C Bransfield, MD, DLFAPA, Videos zu Lyme Disease
(Datum: 7. August 2014)
OnLyme-Aktion.org Online-Petition an den Bundesminister für Gesundheit: Schutz für Patienten mit Borreliose und Co-Infektionen
Aufgrund eines erbitterten Meinungsstreits in der medizinischen Fachwelt und der daraus resultierenden Verunsicherung von Ärzten ist die Versorgung von Patienten mit Borreliose und anderen zeckenübertragenen Infektionen nicht in ausreichendem Maße gewährleistet. Borreliose und Co-Infektionen stellen wegen dieses Streits einen Sonderfall dar, und Patienten sowie ihre behandelnden Ärzte bedürfen deshalb bis zur Klärung dieses Fachdisputs eines besonderen gesetzlichen Schutzes. Europäische Borreliosepatienten fordern deshalb ein Gesetz auf europäischer und auf der jeweiligen nationalen Ebene, das ihre Rechte auf adäquate Therapie garantiert - ähnlich den Gesetzen in den US-Bundesstaaten Vermont (vom 11.3.2014) und New York (Bill number: A7558A).
Durch das Gesetz sollten die folgenden Forderungen realisiert werden:
(Datum: 1. November 2013)
Early spread of Borrelia burgdorferi into mammal tissues, literature review by Marie Kroun
Luft BJ, Steinman CR, Neimark HC, Muralidhar B, Rush T, Finkel MF, Kunkel M, Dattwyler RJ.
Invasion of the central nervous system by Borrelia burgdorferi in acute disseminated infection.
JAMA 1992 Mar 11; 267(10): 1364-7, Erratum in JAMA 1992 Aug 19;268(7):872, Comment in JAMA. 1992 Aug 19;268(7):872; discussion on p 873.
Our findings demonstrate that B. burgdorferi can disseminate to CNS very early in the course of infection with little or no clinical evidence of CNS involvement.
Radiolabeled Borrelia burgdorferi, the etiologic agent of Lyme disease, injected intravenously into rats are cleared from the vasculature within 1 h of injection.
One low passage isolate showed trafficking between the circulation and possibly the vessel walls for the first 2 h after injection.
All strains used were resistant to the effects of normal and heat-inactivated rat serum.
During the first 2 h after injection, B. burgdorferi can be visualized in, and recovered from, the platelet-rich plasma. ... These organisms invade organs (heart, kidneys, bladder, liver, spleen, brain) within 1-6 h after injection.
CONCLUSIONS: The high rate, early onset, and prolonged duration of risk for spirochetemia explain why untreated patients with erythema migrans are at risk for dissemination of B. burgdorferi to anatomic sites beyond the lesion site. Differences in the strain of the infecting spirochete, as well as host factors, may be important determinants of hematogenous dissemination. ... Spirochetemia was not associated with duration of erythema migrans (P > 0.2) or the size of the erythema migrans lesion (P = 0.18), both for the entire study sample (Figure) and separately for those with a single erythema migrans lesion and those with multiple lesions. The oldest lesion associated with spirochetemia was of 33 days duration.
(Datum: 1. Juli 2013)
Bransfield RC, The Psychoimmunology of Lyme/Tick-Borne Diseases and its Association with Neuropsychiatric Symptoms. The Open Neurology Journal, 2012, 6, (Suppl 1-M3) 88-93 1874-205X/12 2012 Bentham Open.
ABSTRACT: Disease progression of neuropsychiatric symptoms in Lyme/tick-borne diseases can be better understood by greater attention to psychoimmunology. Although there are multiple contributors that provoke and weaken the immune system, infections and persistent infections are significant causes of pathological immune reactions. Immune mediated effects are a significant contributor to the pathophysiological processes and disease progression. These immune effects include
and pathophysiological changes have been associated with
Lyme disease has been associated with
Borrelia burgdorferi surface glycolipids and flagella antibodies appear to elicit anti-neuronal antibodies and anti-neuronal antibodies and Borrelia burgdorferi lipoproteins can disseminate from the periphery to inflame the brain.
CONCLUSIONS: Most symptoms associated with Lyme disease and other tick-borne diseases are immune mediated. A progressive sequence of immune effects is associated with a progressive development of cognitive, psychiatric, neurologic, and somatic symptoms. These progressive immune effects include persistent inflammation with cytokine effects, the release of proinflammatory lipoproteins from the outer coat of B. burgdorferi, and autoimmunity.
(Datum: 21. Juni 2013)
Donta ST, Noto RB, Vento JA, SPECT Brain Imaging in Chronic Lyme Disease, Clinical Nuclear Medicine 37, Issue 9, pe219-pe222
Conclusions: Brain SPECT scans are abnormal in most patients with chronic Lyme disease, and these scans can be used to provide objective evidence in support of the clinical diagnosis. The use of certain antibiotic regimens seems to provide improvement in both clinical status and SPECT scans.
(Datum: 30. April 2013)
Michael van den Heuvel, "Lyme-Borreliose: Würfelspiele mit ELISA", DocCheck Newsletter, 29. April 2013 (english)
watch on YouTube
Bei entsprechendem Verdacht untersuchen spezialisierte Labors eine Blutprobe mit Enzyme Linked Immunosorbent Assays (ELISAs) auf Antiäkörper. Das Verfahren hat gleich mehrere Nachteile: Sensitivität, Spezifität und Standardisierung entsprechen nicht der Erwartung. Laut Dr. med. Armin Schwarzbach vom Borreliose Centrum Augsburg bleiben bis zu 70 Prozent aller ELISA-Untersuchungen trotz einer Infektion negativ. "Das Problem ist, dass in den ELISA-Tests zu wenige rekombinante Antigene und Lysate in den falschen beziehungsweise nicht vollständigen Mischungen eingesetzt werden. Wir wissen mittlerweile, dass es zahlreiche neue Borrelien-Subspezies gibt", erklärt Schwarzbach. Problematisch ist die ausgeprägte Antigen-Variabilität und -Varianz einzelner Subspezies.
(Datum: 5. März 2013)
Commonwealth of Massachusetts, "Lyme Disease in Massachusetts,
A Report Issued by the Special Commission to Conduct an Investigation and Study of the Incidence and Impacts of Lyme Disease", February 28th 2013
Education for the Medical Community
1. It is most important that healthcare providers be apprised of the spectrum of Lyme
disease, especially regarding relapsing or persisting symptoms, even after one of two
courses of "standard" antibiotic treatment over a 1-2 month period of time. This condition
may/can be much more frequent than has been previously acknowledged or appreciated,
and the recent (2011) report of the Institute of Medicine (IOM), National Academy of
Sciences (the nation's most highly regarded scientific body) attests to the difficulties
surrounding the diagnosis and management of this complication of Lyme disease
(Critical Needs and Gaps in Understanding Prevention, Amelioration, and Resolution of
Lyme an Other Tick-Borne Diseases: The Short-Term and Long-Term Outcomes:
Workshop Report). Regardless of whether this continued symptomatology is termed post-
Lyme disease or chronic Lyme disease, the cause of the persisting symptoms has yet to
be delineated, and there are currently no tests to determine that the causative organisms
are still present or absent in a given individual; the currently available antibody-based
tests cannot be used to determine that one no longer has, or does have Lyme disease, or to
assess response to treatment. Clinical judgment and assessment of all available
information remain the keys to appropriate management of all patients with Lyme
disease. This point is made by the Centers for Disease Control & Prevention (CDC)
(www.cdc.gov) and is noted on laboratory testing information, yet many physicians
incorrectly rule out Lyme disease solely on the basis of a "negative" lab test.
(Datum: 6. February 2013)
Offener Brief zur katastrophalen Versorgungslage von Borreliose-Patienten, Januar 2013.
"... Viele Ärzte behandeln Borreliose-Patienten höchstens 21 Tage antibiotisch - auch wenn sie bereits am fortgeschrittenen Stadium einer Borreliose leiden. Warum? Weil es bei der Kontroverse zwei "Meinungslager" gibt.
kontakt@OnLyme-Aktion.org
Bitte denken Sie dabei auch an Ihre Freunde, Nachbarn und Verwandte – auch an jene ohne Internet. Es reicht das Einverständnis, dass die Namen unter dem Brief erscheinen dürfen!
(Datum: 19. January 2013)
Sapi E, Kaur N, Anyanwu S, Luecke DF, Datar A, Patel S, Rossi M, Stricker RB (Lyme Disease Research Group, Department of Biology and Environmental Sciences, University of New Haven, New Haven, CT, USA) "Evaluation of in-vitro antibiotic susceptibility of different morphological forms of Borrelia burgdorferi". Infect Drug Resist. 2011;4:97-113. doi: 10.2147/IDR.S19201. Epub 2011 May 3.
Results:
Conclusions:
Antibiotics have varying effects on the different morphological forms of B. burgdorferi. Persistence of viable organisms in round body forms and biofilm-like colonies may explain treatment failure and persistent symptoms following antibiotic therapy of Lyme disease.
(Datum: 26. Dezember 2012)
Lyme disease: issues and hypotheses, a minireview (J. Gruber, editor)
As a result of this interaction we might develop a chronic disease. Our illness becomes an integral part, a new characteristic of us. To fight chronic illness antibiotic therapy needs to be augmented by restoration of our immune-hormone system.
(Datum: 25. Oktober 2012)
Sapi E, Bastian SL, Mpoy CM, Scott S, Rattelle A, et al. (2012) "Characterization of Biofilm Formation by Borrelia burgdorferi In Vitro". PLoS ONE 7(10) e48277. doi:10.1371/journal.pone.0048277 - im Cache
Abstract
(Datum: 14. Oktober 2020)
Borrelia burgdorferi has long been known to be capable of forming aggregates and
colonies. It was recently demonstrated that Borrelia burgdorferi aggregate formation dramatically changes the in vitro
response to hostile environments by this pathogen.
Our results also demonstrated that Borrelia burgdorferi
Analyzing the
extracellular substance of the aggregates for potential exopolysaccharides revealed the existence of both sulfated and non-
sulfated/carboxylated substrates, predominately composed of an alginate with calcium and extracellular DNA present.
Cpn = Chlamydia pneumoniae
W. Webley, PhD, Assistant Professor, University of Massachussetts, Amherst, MA: "Biofilms an Chronic Health Conditions: Challenges for Patients, Doctors and Researchers", Sept. 24, 2009
Chronische Infektionen unterscheiden sich mikrobiologisch wesentlich von akuten Infektionen. Darauf muß die Therapie abgestimmt werden. Im Vortrag werden Parallelen gezogen zwischen Cpn und Bb.
(Datum: 29. Juli 2012)
Dr. Harald Bennefeld, FA für Neurochirurgie/ Sportmedizin, Chefarzt der neurologischen Klinik in Gyhum, Mitglied der Deutschen Borreliose-Gesellschaft e.V.
Vortrag am 29. September 2012 10:30 - 13:00 Uhr, Leipzig
(Datum: 29. Juli 2012)
Deutsche Borreliose-Gesellschaft, Mitteilungen, Juli 2012, Interview vom 8.9.2010 mit Dr. Burgdorfer, Auszug aus der Kurzfassung, Fragen stellten Matthias Jakob und Friedemann Weidner.
Dr. Burgdorfer: Wenn ein Patient von einem Zeckenstich berichtet, dann sollte der Arzt immer an eine Borreliose denken. Und auch wenn die Inkubationszeit vorüber ist, sollte er daran denken, dass vielleicht die Borrelie irgendwo im Gehirn dieses armen Kranken sitzt und hier und da gewisse Schwierigkeiten hervorbringt, die man nicht oder noch nicht definieren kann, weil die Physiologie der Borrelie immer noch so ein großes Rätsel ist.
(Datum: 26. März 2012)
Brian A. Fallon, Elizabeth S. Levin, Pernilla J. Schweitzer, David Hardesty, Inflammation and central nervous system Lyme disease, Neurobiol Dis. 2010 Mar;37(3):534-41 (im Cache).
Sequence homology has been noted between myelin basic protein and B.b. spirochetal flagellin and there are studies demonstrating cross-reactive polyclonal and monoclonal antibodies which recognize flagellar antigenic determinants as well as epitopes on neural cells. Such cross-reactivity could contribute to a chronic, relapsing-remitting, B. burgdorferi- triggered, immune-mediated neurological disorder similar to MS.
(Datum: 29.November 2011)
Lyme Disease Symptoms Pt. 1, Pt. 2, excerpts from P.J. Langhoff, "God Science: The Secret World of Rampant Genetics, Hidden Illness, and Biotech Profiteering", Audio book, Allegory Press LLC, 2011.

zum Vergrößern auf Bild klicken
Quelle: ScienceDirect
Health care providers and individuals exposed to ticks should be aware that transmission of Lyme disease may occur more rapidly than animal models suggest. A diagnosis of Lyme disease should not be ruled out based on a short tick attachment time in a subject with clinical evidence of B. burgdorferi infection.
The attachment time required for a tick to transmit B. burgdorferi, the spirochetal agent of Lyme disease, has important clinical implications. Studies in mice and rabbits suggest that a tick must be attached for at least 36 - 48 h in order for efficient transmission of B. burgdorferi to occur, and these studies have been interpreted to mean that removal of a tick within 36 - 48 h of attachment will prevent transmission of Lyme disease.
Thus the transmission times derived from these studies may not apply to the clinical situation in humans and may give a false sense of security about the risk of Lyme disease following a tickbite.
(Datum: 29.September 2011)
September-Mitteilungen der Deutschen Borreliose-Gesellschaft
Aufruf zur Mitarbeit, Borreliose - eine Multisystemerkrankung, Borreliose-Wahrnehmung, Vermischte Meldungen, Meldepflicht im Saarland, Zecken im städtischen Grün, Fluconazol und Fehlbildungen, Literaturbesprechungen: Pathogenese (Lyme Neuroborreliose), Pathogenese (HGA), Differentialdiagnose Lyme Neuroborreliose vs. Bell's Palsy, Molekularbiologische Diagnostik der Borreliose, Epidemiologie der Borreliose, Ko-Transmission / Ko-Infektion der Zecken.
(Datum: 19.September 2011)
Knauer J, Krupka I, Fueldner C, Lehmann J, Straubinger RK. "Evaluation of the preventive capacities of a topically applied azithromycin formulation against Lyme borreliosis in a murine model." J Antimicrob Chemother. 2011 Sep 15.
Details: Laboratory mice were challenged with Borrelia burgdorferi sensu stricto by needle inoculation or via infected ticks as vectors. Then, an azithromycin-containing formulation was applied once daily to the sites of exposure for three consecutive days. In the case of needle inoculation, a 5% azithromycin formulation was applied starting 1 h, 3 days and 5 days after infection. In the case of tick exposure, 4%, 10% and 20% azithromycin formulations were applied, starting directly after the detachment of the engorged ticks. Concentrations of azithromycin in murine skin were >3800-fold higher than the published minimal inhibitory concentration for B. burgdorferi as soon as 3 h after the first application. After needle inoculation, spirochaetes were not detectable in all infected mice after treatment, if the first application started 1 h or even after 3 days post-infection. Furthermore, no borrelial organisms were detected after topical treatment when ticks were used for spirochaete inoculation.
(Datum: 11. September 2011)
Stellungnahme von Harold Smith (ILADS) zu Lyme Disease Care ("Pennsylvania Lyme Bill" HB272) vor dem Pennsylvania House Human Services Committee, August 30, 2011 (in Unterstützung der HB272). Ein wesentliches Problem sei eine Verzögerung der Diagnose auf Grund fehlender öffentlicher und ärztlicher Vorbildung and ein Verlassen auf Tests, welche nicht ausreichend diagnostisch sind. Am 15 Dezember 2011 hat das Committee dafür gestimmt, HB272 dem "House Floor" zu unterbreiten.
(Datum: 5. Juli 2011)
DBG-Mitteilungen 2011-3
(Datum: 2. April 2011)
Deutsche Borreliose-Gesellschaft: Diagnostik und Therapie der Lyme-Borreliose, Auflage Januar 2011 (Diagnosis and Treatment of Lyme borreliosis, Revised 2nd Edition, Dec 2010)
(Datum: 12. August 2010)
Garth L. Nicolson, Ph.D. (Institute for Molecular Medicine, Huntington Beach, California)
(Datum: 24. Juni 2010)
Uta Everth, "Zielwertfindung und Standards in der Borrelien-Serologie" (Abstract), in "Lyme-Borreliose, Koinfektionen und Multisystemerkrankungen", Deutsche Borreliose-Gesellschaft, Bad Herrenalb, 28. - 30. 5. 2010.
Da man nicht weiß, wer gesund und wer erkrankt ist, weiß man auch nicht, welchen Bruchteil der Erkrankten und welchen der Gesunden der serologische Antikörper-Nachweis erkennt. In diesem Sinn ist die Lage der Testschwelle ("Cut") beliebig, d.h. der Schwelle, jenseits derer der serologische Antikörper-Nachweis eine Person als erkrankt bezeichnet.
(Datum: 26. Mai 2010)
Informationen von Corry Welker
Wie auch Dr. Miklossy, berichtete Dr. Alan MacDonald über seine Untersuchungen, bezüglich Bb und Alzheimer. Er präsentierte Resultate und Hypothesen auf eine Tagung der LDA+ILADS in Philadelphia. Der Originaltext des Interviews datiert aus April 2008.
Bericht von Paul Christensen auf www.canlyme.com
Webseite Dr MacDonald
Die Risikogebieten sind unverändert geblieben:
Gebiete mit Einzelfällen in der Vergangenheit werden beobachtet.
Weitere Zahlen und Werte zu den einzelnen Landkreisen und jeweiligen Bundesländern von 2002 bis 2009 finden Sie bei: http://www.rki.de/cln_160/nn_1759378/DE/Content/Infekt/EpidBull/Archiv/2010/17__10__Anlage__
Tabelle,templateId=raw,property=publicationFile.pdf/17_10_Anlage_Tabelle.pdf (14 Seiten)
(Datum: 1. September 2009)
B Pawlicki, The Use of Silver Hydrosol in Treating Neurological Lyme Disease
Medication:
After improvement of health status: Maintenance therapy with
(Datum: 23. Juli 2009)
Informationen der Deutschen Borreliose-Gesellschaft
Results: Of 392 patients suspected of having neuro-Lyme disease,
66 patients proved to have the disease on the basis of clinical criteria, serologic results, and response to treatment.
Of the 7 patients with foci of T2 prolongation in the white matter, 3 were an age at which white matter findings due to small-vessel disease are common.
Conclusion: In cases of nerve-root or meningeal enhancement, Lyme disease should be considered in the differential diagnosis in the proper clinical setting.
Results: The majority (61%) of patients in this case series were diagnosed with early Lyme disease. Of those diagnosed with early Lyme disease, 13% did not present with erythema migrans; of those not presenting with a rash,
54% had been previously misdiagnosed. Among those with a rash, the diagnosis of erythema migrans was initially missed in 23% of patients whose rash was subsequently confirmed. Of all patients previously misdiagnosed, 41% had received initial antibiotics likely to be ineffective against Lyme disease.
(Datum: 19. Mai 2009)
Informationen von Corry Welker
Quelle: Zecken durch Klimawandel gefährlicher: Verschiebung der Jahreszeiten macht Erreger hartnäckiger, Pressetext Austria.
Gatewood AG, Liebman KA, Vourc'h G, Bunikis J, Hamer SA, Cortinas R, Melton F, Cislo P, Kitron U, Tsao J, Barbour AG, Fish D, Diuk-Wasser MA., Climate and tick seasonality are predictors of Borrelia burgdorferi genotype distribution. Appl Environ Microbiol. 2009 Apr;75(8):2476-83. Epub 2009 Feb 27.
Das RIVM hat in 2007 und 2008 mit 300 Hausärzten bei circa 700 Teilnehmern die Daten bzw. Zeckenstiche + Sera untersucht. 42% der Personen stellten sich beim Arzt wegen EM vor und 58% wegen stattgefundener Stiche. Es wurden 323 bei den Teilnehmern entfernte Zecken untersucht. Die meisten davon waren Ix. ricinus-Zecken. 55% waren Nymphen; 44% adulte zecken und nur 1% war Larven.
Borrelien 22%, davon B afz 16%, Bgar 4%; Bbss 2%; B valais 1%
Rickettsien 22%
Ehrlich/Anapl 10%
Babesien 4%
Min. 1 Infektion 46%
Mehrfach infiziert 12%
Mehrere Borr. Typen 5%
Mit diesem Beitrag stellt sich das BCA der Diskussion um die Notwendigkeit und Berechtigung der Langzeit-Antibiose, gegenüber der gerade viele Hausärzte noch erhebliche Vorbehalte haben. Leider noch zu unbekannt im deutschsprachigen Raum sind klinische Studien aus den letzten Jahren, die den Erfolg dieser Langzeit-Antibiose beweisen. Zu diesem Zweck werden in diesem Beitrag beispielhaft die Ergebnisse des renommierten Prof. Dr. med. Sam T. Donta, dem Direktor der Abteilung für Infektionskrankheiten und Biomolekular-Medizin - Bereich Lyme-Borreliose am Boston University Medical Center, aus dessen Studie von 2003 mit 239 Lyme-Borreliose Patienten dargestellt. Diese Studie unterlegt die Berechtigung der vom BCA durchgeführten Langzeit-Antibiosen und dass die chronische Lyme-Borreliose ein zu behandelndes Krankheitsbild ist.
(Datum: 3. März 2009)
(Datum: 13. February 2009)
(Datum: 24. Oktober/2. November 2008)
Deutsche Borreliose-Gesellschaft
Mitglieder der Arbeitsgruppe der Empfehlungen:
Prof. Dr. med. Rüdiger von Baehr FA für Innere Medizin Institut für medizinische Diagnostik, Berlin - PD Dr. med. Walter Berghoff FA für Innere Medizin, Rheinbach - Dr. med. Harald Bennefeld FA für Neurochirurgie, Sportmedizin, Heinrich Mann Klinik Bad Liebenstein - Hans-Peter Gabel FA für Allgemeinmedizin, Wolfenbüttel - Prof. Dr. med. Fred Hartmann FA für Innere Medizin, Chefarzt a. D., Ansbach - Dr. med. Wolfgang Heesch FA für Innere Medizin, Vellmar - Dr. med. Gabriele Herrmann FÄ für Orthopädie, Berlin - Dr. med. Petra Hopf-Seidel FÄ für Neurologie und Psychiatrie sowie FÄ für Allgemeinmedizin, Ansbach - Dr. med. Bernd-Dieter Huismans FA für Innere Medizin, Umweltmedizin, Crailsheim - Dr. med. Wolfgang Klemann FA für Innere Medizin, Pforzheim Dr. med. Uwe Neubert FA für Dermatologie, Dermatologische Klinik LMU München, Akad. Direktor i. R. - Dr. med. Andrea Roczinski FÄ für Allgemeinmedizin, Königslutter - Dr. med. Armin Schwarzbach FA für Laboratoriumsmedizin, Augsburg - Dr. med. Barbara Weitkus FÄ für Kinderheilkunde, Berlin - Cord Uebermuth FA für Augenheilkunde, Düsseldorf Dr. med. Jochen Viebahn FA für Allgemeinmedizin, Gummersbach - Dr. med. Peter Voss FA für Allgemeinmedizin, Ulm
ABSTRACT
BACKGROUND:
The long latent stage seen in syphilis, followed by
chronic central nervous system infection and inflammation, can be explained by
the persistence of atypical cystic and granular forms of Treponema pallidum. We
investigated whether a similar situation may occur in Lyme neuroborreliosis.
METHOD:
Atypical forms of Borrelia burgdorferi spirochetes were induced exposing
cultures of Borrelia burgdorferi (strains B31 and ADB1) to such unfavorable
conditions as osmotic and heat shock, and exposure to the binding agents
Thioflavin S and Congo red. We also analyzed whether these forms may be induced
in vitro, following infection of primary chicken and rat neurons, as well as rat
and human astrocytes. We further analyzed whether atypical forms similar to
those induced in vitro may also occur in vivo, in brains of three patients with
Lyme neuroborreliosis. We used immunohistochemical methods to detect evidence of
neuroinflammation in the form of reactive microglia and astrocytes.
RESULTS:
Under these conditions we observed atypical cystic, rolled and granular forms of
these spirochetes. We characterized these abnormal forms by histochemical,
immunohistochemical, dark field and atomic force microscopy (AFM) methods. The
atypical and cystic forms found in the brains of three patients with
neuropathologically confirmed Lyme neuroborreliosis were identical to those
induced in vitro. We also observed nuclear fragmentation of the infected
astrocytes using the TUNEL method. Abundant HLA-DR positive microglia and GFAP
positive reactive astrocytes were present in the cerebral cortex.
CONCLUSION:

Figure 7. Extra- and intracellular atypical and cystic forms of spirochetes in the cerebral cortex of a patient with pathologically and serologically confirmed chronic Lyme neuroborreliosis where Borrelia burgdorferi sensu stricto was cultivated from the brain.
(Datum: 28. August 2008)
(Datum: 9. Juli 2008)
Background: The Panel assigned to hear Dr. Jones' case completed their review of the evidence presented over the course of 11 days of hearings that had begun on March 28, 2006, and handed down recommendations. If these recommendations were accepted by the Medical Licensing Board, Dr. Jones would be fined $10,000, and be subjected to having his patient care monitored by a physician for a period of two years. The process would be put into place within 60 days, with the monitoring physician reporting back to the Medical Board periodically. The attorneys had the opportunity to submit briefs and to provide oral arguments to the Medical Licensing Board at their monthly meeting. The Board would then decide whether to affirm the findings of the panel, to dismiss it, or to modify it in some way. Their findings would be binding on Dr. Jones, unless the ruling was overturned on some level of the appeal process.
(Datum: 17. Juni 2008
Corry Welker informiert:
Der Pharma-Großhandel listet den Test edv-mäßig unter "MEDtest Zecken/Borreliose".
Aussagekraft: Der Test springe an bei ca. 300 Borrelien im Markierungsfeld, was wohl 30% Infektionsgefahr bedeute, sagte man mir. Weitere Info folgt.
MEDtest ist das Gesundheitszentrum+ München, Rainfarn-Apotheke&Sanitätshaus, Rainfarnstr 36 in D-80935 München, Tel.: (089) 312 023 01, wo man aber nur Packungen mit 100 Stück liefere an Praxen, Kliniken, Pharma-Großhandel etc.
Ein Vorzeige-Exemplar wurde mir für die SHG zugesagt. Diesbezüglich und Details kann man nachfragen bei Herrn Grundmann oder Dr. Helm, Gesundheitszentrum+ München, 089 - 312 023 01.
Von einer Arbeitsgruppe der Deutschen Borreliose-Gesellschaft mit folgenden Mitgliedern verfasst: R. von Baehr, W. Berghoff, H. Bennefeld, H.-P. Gabel, F. Hartmann, W. Heesch, G. Herrmann, P. Hopf-Seidel, B.-D. Huismans, W. Klemann, U. Neubert, A. Roczinski, A. Schwarzbach, B. Weitkus, C. Uebermuth, J. Viebahn, P. Voss
Diese Empfehlungen wurden im Rahmen der Jahresversammlungen 2006 und 2007 der BorrelioseGesellschaft von Mitgliedern der Arbeitsgruppe vorgestellt. Kritische Hinweise und Ergänzungen wurden in diesen Empfehlungen berücksichtigt. Die vorliegende Fassung entspricht dem Stand der Diskussion vom Februar 2008. Diese Empfehlungen werden weiter diskutiert und aktualisiert werden.
"Borreliose erkennen und wirksam behandeln" ist aus schulmedizinischer und ganzheitlicher Sicht geschrieben mit breitgefächerten Informationen. Neben ausführlicher Info über Zecken, vermittelte Erreger und Begleiterkrankungen handelt fast die Hälfte des Buches über Symptomatik, Diagnostik und Therapie der chronischen Borreliose mit Empfehlungen für verschiedene Antibiotika. Im Anhang gibt es Adressen, Glossar und einen ausführlichen Index.
In neuropsychologischen Tests sind nach Literaturangaben die Defizite objektivierbar. Das EEG und der Liquor cerebrospinalis sind fast immer normal (im Vergleich zur europäischen Literatur erstaunt das regelhafte Fehlen entzündlicher Liquorveränderungen einschließlich einer intrathekalen spezifischen Antikörpersynthese zum Zeitpunkt der Diagnosestellung). Im MRT können zum Teil "white mater lesions" gefunden werden. Unter antibiotischer Therapie seien bei einem Teil der Patienten eine Besserung der Klinik, neuropschych. Testresultate sowie der Befunde im SPECT zu beobachten.
Siehe dazu auch: Blanc F, Jaulhac B, Fleury M et al., Relevance of the antibody index to diagnose Lyme neuroborreliosis among seropositive patients. Neurology. 2007 Sep 4;69(10):953-8
(Datum: 20. Mai 2008)
Raphael B. Stricker, Infectious Diseases Society of America (IDSA) Lecture, Counterpoint: Long-Term Antibiotic Therapy Improves Persistent Symptoms Associated with Lyme Disease, Clinical Infectious Diseases 2007;45:149-157
Pay per Article - Login: US $15.00
Methods: Review of the pathophysiology of B. burgdorferi infection and the peer-reviewed literature on diagnostic Lyme disease testing, standard treatment results, and coinfection with tickborne agents, such as Babesia, Anaplasma, Ehrlichia, and Bartonella species. Examination of uncontrolled and controlled trials of prolonged antibiotic therapy in patients with persistent symptoms of Lyme disease.
Results: The complex "stealth" pathology of B. burgdorferi allows the spirochete to invade diverse tissues, elude the immune response, and establish long-term infection. Commercial testing for Lyme disease is highly specific but relatively insensitive, especially during the later stages of disease. Numerous studies have documented the failure of standard antibiotic therapy in patients with Lyme disease. Previous uncontrolled trials and recent placebo-controlled trials suggest that prolonged antibiotic therapy (duration, >4 weeks) may be beneficial for patients with persistent Lyme disease symptoms. Tickborne coinfections may increase the severity and duration of infection with B. burgdorferi.
(Datum: 15. Mai 2008)
M.K. Viljanen (Turku Immunology Centre, Finland), Host Defence in Lyme Borreliosis
One of the most debated questions in Lyme
borreliosis research is pathogenesis of antibiotic
treatment resistant disease manifestations. Two main
hypotheses presented to explain this phenomenon
are persistent infection and infection-induced
autoimmunity. We have succeeded in establishing
a much-needed animal model for this disease
entity (Yrjänäinen et al., submitted). Our results show
that the presence of vegetative spirochetes is no
prerequisite for the persisting symptoms. However,
using this model we have found out that when the
mice receive immunosuppressive treatment with
anti-TNF-alpha after a latent period of several weeks,
borreliae are activated from a dormant state and
the animals develop spirochetemia (Yrjänäinen et al.,
manuscript in preparation). Thus, our results support
the persistent infection hypothesis.
more:
Correspondence: Stricker RB, J Infect Dis. 2008 May 1;197(9):1352-3
Ältere
Bekanntmachungen. Sie wurden von hier z.T.
verlagert.